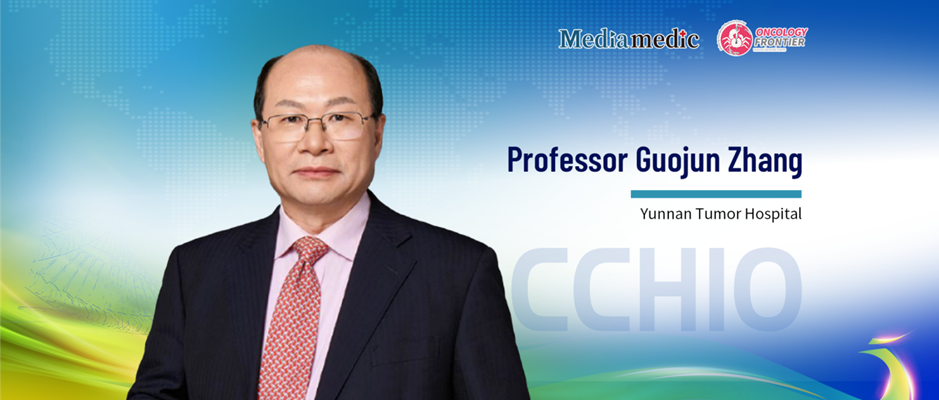
Integrating Chinese and European Wisdom to Explore New Frontiers in Cancer Control — Review of the CACA–EACR Session at the 2025 CCHIO Conference
Editor’s Note: The 2025 China Conference on Holistic Integrative Oncology (CCHIO), jointly organized by the Chinese Anti-Cancer Association (CACA) and the Tengchong Scientist Forum Organizing Committee Office, and co-hosted by…