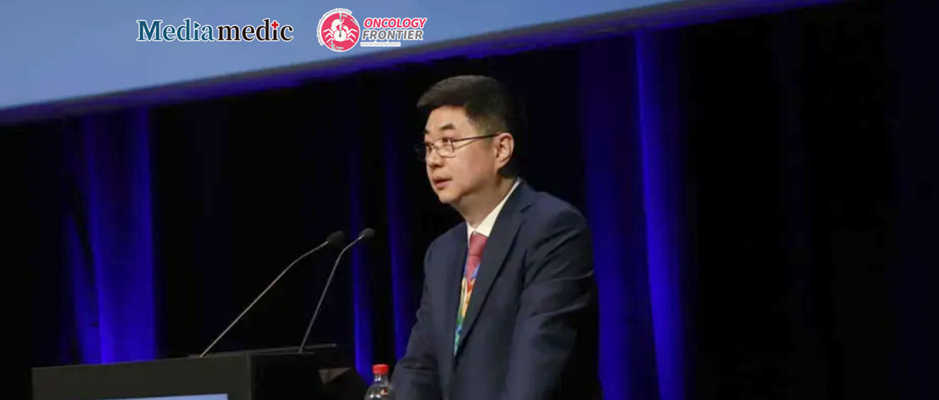
Editor’s Note At the ESMO 2025 Congress, Prof. Kun Wang from Guangdong Provincial People’s Hospital delivered an oral presentation reporting results from a prospective phase III trial exploring the relationship between pegfilgrastim administration timing and bone pain. The study addressed the persistent challenge of managing pegfilgrastim-induced bone pain following taxane chemotherapy and innovatively examined whether delayed dosing could reduce this adverse effect.
The findings demonstrated that administering pegfilgrastim 72 hours after chemotherapy significantly reduced both the incidence and severity of bone pain without compromising its neutrophil-protective efficacy. To discuss the study’s clinical motivation, implications for patient quality of life, and how this “China strategy” may inform global supportive care, Oncology Frontier invited Prof. Wang for an in-depth conversation.
Oncology Frontier: In clinical practice, what specific observations or reflections prompted your team to design this prospective randomized study on pegfilgrastim dosing timing and bone pain? Could you share the background and rationale behind the research?
Prof. Kun Wang: In daily practice, we observed that patients receiving taxane-based chemotherapy frequently report musculoskeletal and bone pain. Because chemotherapy often leads to febrile neutropenia, these patients routinely receive prophylactic pegfilgrastim (a long-acting G-CSF). However, many patients experience noticeable bone pain after injection—sometimes even worse than the chemotherapy-induced discomfort itself—significantly affecting their quality of life.
We explored various methods to relieve this pain, but none were particularly effective. That led us to a simple question: Could adjusting the timing of pegfilgrastim administration help alleviate pain more effectively? Based on this idea, we designed a prospective randomized controlled trial to test the hypothesis.
According to NCCN guidelines, pegfilgrastim may be administered within 1–4 days after chemotherapy. In real-world clinical practice, however, most physicians prefer 24–48 hours post-chemotherapy. Therefore, we established three dosing schedules—24, 48, and 72 hours—to compare the effects of different timings on bone pain intensity and other adverse events. Our goal was to identify a more optimal, patient-friendly strategy to reduce pain and enhance treatment tolerance.
Oncology Frontier: What were the key findings of the study? How do you think these results will impact supportive care strategies and quality of life for breast cancer patients?
Prof. Kun Wang:
We enrolled stage I–III breast cancer patients at intermediate or high risk of neutropenia and randomized them (1:1:1) into the 24-hour, 48-hour, and 72-hour groups.
The primary endpoint was the area under the curve (AUC) of worst daily bone pain scores (0–10 numeric rating scale) over the first five days of the initial chemotherapy cycle. Secondary endpoints included the incidence and duration of severe bone pain (NRS >5), as well as the incidence of neutropenia and febrile neutropenia.
A total of 159 patients were included in the intention-to-treat analysis (53 per group).
- In the first chemotherapy cycle, the mean AUC for bone pain was significantly lower in the 72-hour group (6.05; 95% CI: 3.91–8.19) than in the 24-hour (12.74; 95% CI: 10.60–14.88) and 48-hour (14.20; 95% CI: 12.06–16.34) groups.
- The pain curve from day 1 to day 5 clearly showed that patients in the 72-hour group reported markedly lower pain intensity than those in the other two groups.
- The incidence of severe bone pain fell dramatically from 58.5% (24-hour) and 66.0% (48-hour) to 22.6% (72-hour).
- The average duration of severe bone pain decreased from 1.08 days and 1.42 days to 0.34 days, respectively.
- No significant differences were observed between the 24-hour and 48-hour groups.
- Rates of neutropenia were similar across groups, and no febrile neutropenia cases occurred.
In summary, compared with administration at 24 or 48 hours after chemotherapy, 72-hour pegfilgrastim dosing significantly reduced the incidence and severity of bone pain while maintaining full hematologic efficacy.
Oncology Frontier: Based on your experience and this study’s findings, what is your recommendation for pegfilgrastim administration timing? Do you believe this could influence future clinical guidelines? What are the next research directions, such as validation in other regimens or cancers, or optimizing bone pain management strategies?
Prof. Kun Wang: Based on our results, for patients receiving taxane-based chemotherapy who are at risk for neutropenia, we recommend delaying pegfilgrastim administration to 72 hours post-chemotherapy. This approach significantly reduces bone pain without affecting other adverse events. It is a simple, cost-effective, and patient-centered strategy that could meaningfully improve comfort and treatment adherence.
Looking forward, several directions merit further study:
- Expanding validation across different tumor types, age groups, and disease stages (early, intermediate, advanced).
- Investigating whether similar timing benefits apply after non-taxane chemotherapy, such as anthracycline-based regimens.
- Further refining bone pain management strategies by integrating pharmacologic and non-pharmacologic interventions.
We hope these findings will inspire guideline updates and promote a more evidence-based, patient-friendly approach to supportive care in oncology.
Prof. Kun Wang

Vice President, Cancer Hospital, Guangdong Provincial People’s Hospital