Editor’s note:
Systemic treatment can extend the overall survival of patients with advanced hepatocellular carcinoma (HCC). However, results vary among individuals, and the predictive factors for survival rates in advanced HCC patients are still unclear. Previous studies have shown that the patient’s frailty index is related to adverse outcomes in liver cirrhosis and liver transplant recipients. It has also been confirmed to predict the results of systemic treatment in cancer patients. From September 7-9, 2023, the 17th Annual Meeting of the International Liver Cancer Association (ILCA) was grandly held in Amsterdam, the Netherlands. At this ILCA 2023 meeting, Dr. Karen W.D. Prince from the Prince Alfred Hospital in Sydney, Australia, delivered an oral report on a multicenter prospective observational study (Abstract No.: O-08), which analyzed the factors related to the mortality rate of advanced HCC patients undergoing systemic treatment. The results show that the Liver Frailty Index (LFI) can serve as an independent predictor of mortality in late-stage HCC patients undergoing systemic treatment. This journal provides a comprehensive report.
Muscle atrophy, malnutrition, and declining liver function are common clinical features in patients with chronic liver disease and cirrhosis. This results in the combined formula of serum sodium with the end-stage liver disease model (MELD-Na) score failing to accurately predict the mortality of cirrhosis patients. In 2017, a study by Jennifer C. Lai and others was published in the journal Hepatology, where they used the frailty index to screen for extrahepatic complications in patients with cirrhosis. They found that the frailty index can improve the prediction of mortality in patients with cirrhosis (see Figure 1).

Figure 1. The predicted survival probability of four categories of cirrhosis patients on the liver transplant waiting list based on MELDNa and frailty index scores.
Frailty is also a state susceptible to internal imbalances, such as manifestations after chemotherapy or cancer surgery. The Ann Oncol journal published a systematic review article observing the correlation between frailty indices and clinical outcomes in elderly cancer patients with different stages of solid tumors or hematologic malignancies. The results showed that more than half of the elderly cancer patients have pre-frailty or frailty, and these patients have a significantly increased risk of chemotherapy intolerance, postoperative complications, and mortality (see Figure 2).

Figure 2. The relationship between frailty, pre-frailty, and mortality in elderly cancer patients (adjusted data).
At the ILCA 2023 conference, Dr. Karen W.D. Prince reported on this international multicenter, prospective, observational cohort study. It included adult HCC patients who started systemic treatment from 2019-2022. Frailty was assessed using the Liver Frailty Index (LFI) and categorized based on the predefined categories of advanced liver disease. The primary endpoint was overall survival; secondary endpoints were disease progression, adverse events, and drug discontinuation. The Cox proportional hazard was used for univariate effects and subsequent multivariate modeling, using backward stepwise regression to estimate event time analysis. The Liver Frailty Index (LFI) was defined as a continuous categorical variable, using predefined cutoff values to explore the best LFI threshold value related to the primary endpoint.
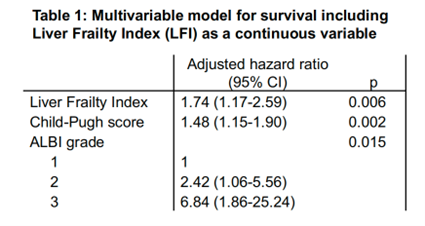
The study included a total of 102 patients, of which 80% were male with a median age of 67 years (IQR 60-73). Most had viral hepatitis (HCV 39%, HBV 29%), Child-Pugh A (75%), ECOG 0-1 (89%), and BCLC C stage (59%). The proportions of patients receiving tyrosine kinase inhibitors (54%) and immune checkpoint inhibitors (46%) were similar. Other baseline clinical features were comparable across the three groups of pre-frailty, frailty, and healthy, except for a higher proportion of ECOG 2/3 in the frailty group (P=0.002). The median LFI was 4.13 (IQR 3.81-4.43): 75% were pre-frail, 22% were frail, and 4% were healthy. After adjusting for Child-Pugh scores and ALBI grades, LFI was independently associated with patient survival (aHR=1.74, 95%CI: 1.17-2.59, P=0.006), as seen in Table 1.
Table 1. Multifactorial survival model including the Liver Frailty Index (LFI) as a continuous variable.
The best survival cutoff value at 1 year was LFI 4.2 (AUC 0.658), which was significant in both univariate and multivariate analyses predicting death (Figure 3).
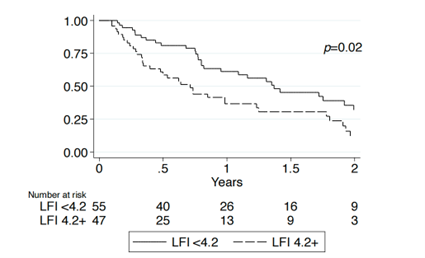
Figure 3. Survival curve analysis through the most predictive 1-year frailty threshold (LFI=4.2).
Although the incidence rates of disease progression and adverse events were similar, the analysis indicated that frailty was significantly associated with early discontinuation of systemic treatment; moreover, discontinuation due to declining liver function was more common in frail patients. The results remained consistent even after further excluding patients with Child-Pugh B8 or ECOG 2 and above. In summary, this study suggests that in HCC patients receiving systemic treatment, frailty is an independent predictor of death.
References:
1. Lai JC, Covinsky KE, Dodge JL, et al. Development of a novel frailty index to predict mortality in patients with end-stage liver disease. Hepatology. Aug 2017;66(2):564-574. doi:10.1002/hep.29219.
2. Handforth C, Clegg A, Young C, et al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol. Jun 2015;26(6):1091-1101. doi:10.1093/annonc/mdu540.
3. Karen Waller David Prince, Miriam Levy, et al. The Liver Frailty Index Is An Independent Predictor Of Mortality In Patients With Advanced Hepatocellular Carcinoma Undergoing Systemic Therapy: A Multicentre, Prospective Observational Study. ILCA 2023 Abstract O-08
TAG: ILCA 2023, Commentary, HCC

