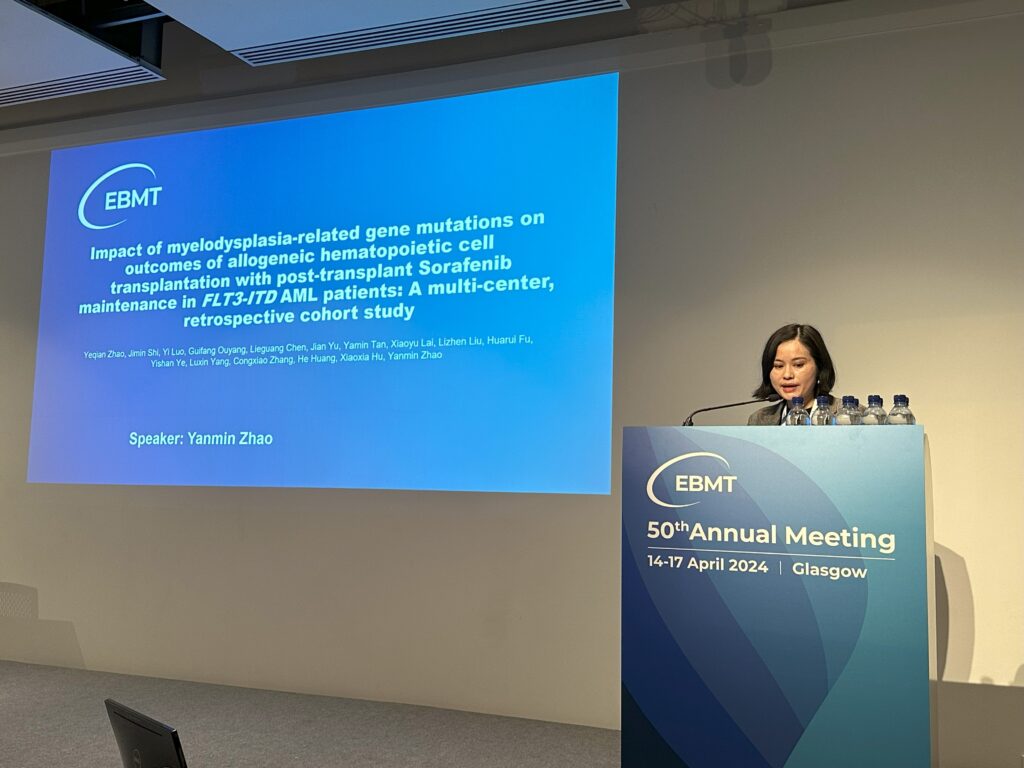
Editor’s note: FMS-like tyrosine kinase 3 (FLT3) mutations, particularly internal tandem duplication mutations (FLT3-ITD), are one of the significant factors affecting the prognosis of patients with acute myeloid leukemia (AML). Overcoming the challenge of relapse after transplantation in patients with FLT3-mutated AML remains a significant clinical hurdle. At the 50th European Bone Marrow Transplantation (EBMT) annual meeting, Professor Yanmin Zhao from The First Affiliated Hospital of Zhejiang University School of Medicine presented a study (Abstract No.: OS18-08), which explored the impact of mutations in myelodysplasia-related (MR) genes on maintenance treatment outcomes after transplantation for FLT3-ITD AML patients. “Oncology Frontier – Hematology Frontier” invited Professor Yanmin Zhao to share insights into the maintenance treatment strategies, challenges, and future research directions for FLT3-ITD mutant AML patients after transplantation.
Professor Yanmin Zhao delivered an outstanding presentation at the EBMT conference.
The continuous development of diagnostic and therapeutic technologies has improved the prognosis for FLT3-ITD mutant AML patients.
FLT3-ITD mutation is a common genetic mutation type among AML patients, typically associated with a poor prognosis. Compared to patients with wild-type FLT3, those with FLT3-ITD mutation have lower rates of treatment remission, shorter remission periods, and higher relapse rates. The prognosis of FLT3-ITD mutant AML is linked to several factors, including the number of ITDs, insertion sites, insertion length, and allelic ratios, among other characteristics of the FLT3 mutation. Coexisting gene mutations also influence the prognosis of FLT3-ITD mutant AML patients. For instance, FLT3-ITD mutant AML patients with an NPM1 mutation generally have a better prognosis, whereas those with additional mutations in IDH1/2, TET2, DNMT3A, WT1, or both NPM1 and DNMT3A have poorer outcomes. During the disease progression of FLT3-mutated AML, clonal evolution may lead to the loss or acquisition of new FLT3 mutations, affecting patient outcomes. FLT3 inhibitors, such as midostaurin, gilteritinib, and quizartinib, have shown promising therapeutic effects and have improved the prognosis of AML patients to some extent. Results from the QuANTUM-First trial indicated that quizartinib combined with chemotherapy improves overall survival for FLT3-ITD mutant AML patients, offering a new and tolerable treatment option for newly diagnosed adult patients with this mutation.
At this EBMT conference, Professor Yanmin Zhao reported on a study by her team, which found an increased relapse rate among FLT3-ITD mutant AML patients. However, with continuous improvements in hematopoietic stem cell transplantation techniques and the advent of more targeted drugs, the survival of these patients has significantly improved. Therefore, the previously perceived high relapse rates post-transplantation for FLT3-ITD mutant patients are being effectively addressed.
Maintenance Treatment Strategies for FLT3-ITD Mutant AML Patients After Transplantatio
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a key treatment for AML patients to achieve long-term survival. However, FLT3-ITD mutant AML patients face a high risk of relapse after transplantation, posing a significant challenge for clinical treatment. The emergence of FLT3 inhibitors and other targeted drugs provides new strategies to reduce post-transplant relapse.
In terms of maintenance treatment after transplantation, several studies have confirmed that tyrosine kinase inhibitors (TKIs) and FLT3 inhibitors effectively reduce the relapse rate of FLT3-ITD mutant AML patients. Particularly, sorafenib, an effective FLT3 inhibitor, has shown potential in extending the relapse-free survival period in post-transplant maintenance treatment. Therefore, it is recommended to initiate maintenance treatment with FLT3 inhibitors like sorafenib as early as possible after transplantation.
For patients who cannot receive drug therapy, donor lymphocyte infusion (DLI) is also an effective treatment method. Studies have shown that DLI can reduce the relapse risk and improve survival rates for FLT3-ITD mutant patients. Additionally, the formulation of individualized treatment strategies is equally important to enhance treatment efficacy, possibly requiring a combination of drug maintenance treatment, DLI, and other feasible treatment approaches.
With ongoing advances in medical research, the future holds promise for more innovative treatment methods that could further reduce the post-transplant relapse risk and improve overall outcomes for FLT3-ITD mutant AML patients. Currently, clinicians and researchers are dedicated to developing and optimizing post-transplant maintenance treatment protocols to provide more precise and effective treatment options for AML patients.
MR gene mutations may be associated with poor outcomes in FLT3-ITD mutant AML patients
In the field of AML treatment, FLT3 mutations are a critical prognostic factor, and the introduction of FLT3 inhibitors has significantly improved treatment outcomes for patients with FLT3-mutated AML. However, even after treatment with FLT3 inhibitors and allo-HSCT, some patients still face the risk of relapse. At this EBMT conference, Professor Yanmin Zhao’s team presented a study aimed at identifying specific subgroups among FLT3-ITD mutant AML patients undergoing sorafenib maintenance treatment who experience worse outcomes, to further understand the clinical and molecular characteristics leading to post-transplant relapse, thereby providing more precise treatment strategies for this high-risk patient group.
This multicenter retrospective cohort study included AML patients who underwent allo-HSCT between January 2016 and December 2022 at three hospitals. Inclusion criteria were: (1) aged 14-70 years, (2) confirmed diagnosis of FLT3-ITD mutant AML, (3) achieved complete remission (CR) post-transplant and subsequently received sorafenib as part of their maintenance treatment. Comprehensive screening for cytogenetic features and accompanying gene mutations was conducted to identify genetic risk factors affecting the prognosis of FLT3-ITD mutant AML patients. A total of 171 patients were included, with results showing a 2-year overall survival (OS) rate of 85.5% (95% CI: 80.0%-91.3%), and a 2-year relapse-free survival (RFS) and cumulative incidence of relapse of 79.1% (95% CI: 72.8%-86.0%) and 20.3% (95% CI: 14.7%-27.6%), respectively. Among patients in CR at the time of transplantation, there was no difference in prognosis between those with negative minimal residual disease (MRD) and those with positive MRD (2-year OS: 88.70% vs. 83.30%, P=0.930). Multivariable analysis using a Cox regression model showed that mutations in myelodysplastic-related (MR) genes were independently associated with a poor prognosis (OS: HR 11.51, 95% CI: 1.44-91.80, P=0.021; RFS: HR 2.50, 95% CI: 1.09-5.80, P=0.031). Additionally, DNMT3A mutations were also identified as an independent risk factor affecting RFS (HR 2.7, 95% CI: 1.30-5.60, P=0.008). Interestingly, in the 2022 European LeukemiaNet high-risk group (ELN2022), patients carrying MR gene mutations showed significantly worse OS and RFS compared to those without mutations, while high-risk ELN2022 patients without MR gene mutations had survival outcomes comparable to the medium-risk control group.
The results of this study indicate that in patients who achieve remission, the MRD status, whether negative or positive, does not impact the risk of post-transplant relapse and transplant outcomes. However, for patients with positive MRD, especially those with additional gene mutations such as DNMT3A mutations, a higher relapse rate and lower relapse-free survival were observed. This finding suggests that post-transplant treatment strategies need to pay particular attention to patients carrying additional high-risk gene mutations.
The significance of this study lies in not only revealing the molecular basis for post-transplant relapse in patients with FLT3-mutated AML but also providing important references for future personalized treatment. For patients carrying specific gene mutations, more intensified treatment strategies, such as adjusting FLT3 inhibitor usage, employing donor lymphocyte infusions, or exploring new targeted treatment approaches, may need to be considered. These findings are crucial for optimizing clinical treatment decisions and improving patient outcomes.
Future Directions in FLT3-Mutated AML Treatment: Personalized Therapy and Integrated Management Strategies
In the clinical treatment of AML, the development of targeted therapies for FLT3 mutations has significantly improved survival benefits for patients. However, there remain critical unmet clinical needs and challenges, particularly for patients with FLT3-mutated AML who undergo allo-HSCT. First, the issue of relapse in a subset of patients needs to be addressed more clearly, especially understanding the mechanisms of relapse in patients carrying multiple MR gene mutations. It is crucial to delve deeper into the subclonal typing and clonal evolution of their leukemia clones to reveal the molecular mechanisms of relapse. Another goal is to better balance the graft-versus-host disease (GVHD) and graft-versus-leukemia (GVL) effects post-transplant. During FLT3 inhibitor treatment, balancing the GVHD and GVL effects to enhance therapeutic efficacy without increasing the risk of GVHD remains a challenging problem that needs further breakthroughs. Additionally, we anticipate more supplemental data on the efficacy of new drugs, including FLT3 inhibitors like gilteritinib and other novel drugs in preventing relapse, as well as head-to-head studies comparing the efficacy and safety of different TKIs. Future treatments will increasingly be based on the molecular genetic characteristics of patients, aiming for personalized treatment plans to achieve precision medicine. There is also a need to strengthen the exploration of integrated treatment plans, including induction chemotherapy, allo-HSCT, post-transplant interventions, and combination therapies involving different drugs such as FLT3 inhibitors with demethylating agents and immunomodulators to improve response rates and maximize therapeutic effects. Overall, the treatment strategies for FLT3-mutated AML are gradually transitioning towards precision medicine, and future research will focus more on optimizing personalized and integrated treatment plans to provide more effective and less side-effect-prone treatment options for patients.
Under the leadership of Professor Huang He, Professor Yanmin Zhao’s team has also been committed to exploring hematopoietic stem cell transplantation and cellular immunotherapy in the treatment of hematological diseases, particularly focusing on complications related to hematopoietic stem cell transplantation, such as GVHD and post-transplant relapse. Balancing the GVHD and GVL effects and making better use of numerous new drugs (including targeted and immunotherapeutic drugs) to bring about better transplant outcomes for patients is a continual effort by Professor Zhao’s team. We also look forward to the release of more significant research data in the future, which will provide better clinical references for diagnostic and therapeutic decisions and patient choices.
Expert Profile

Professor Yanmin Zhao
Medical Doctor, Chief Physician, PhD Supervisor, Distinguished Researcher
Vice Director of the Hematopoietic Bone Marrow Transplantation Center at the First Affiliated Hospital, Zhejiang University School of Medicine
Youth Committee Member of the Hematological Tumors Committee, Chinese Anti-Cancer Association
Committee Member of the Hematopoietic Stem Cell Transplantation and Cellular Therapy Committee, China Medical Pharmaceutical Education Association
Vice Chair of the Youth Committee of the Hematology Branch of the Zhejiang Provincial Medical Association
Zhejiang Excellent Young Scholar of the Immunology Society of Zhejiang
Secretary of the Clinical Trial Hematology Group at the First Affiliated Hospital, Zhejiang University School of Medicine
Recipient of the Zhejiang Provincial Top-level Health Talents (551 Talent Plan). Principal investigator for one project supported by the National Natural Science Foundation of China for Young Scientists, and three general projects. Key researcher for the National Key R&D Program.
Editorial board member of the journal Cell Transplantation, and has published over 40 SCI papers as the first author or corresponding author in journals including the Journal of Hematology & Oncology, JAMA Network Open, and American Journal of Hematology. Has delivered oral presentations multiple times at international conferences such as ASH, EHA, EBMT, and APBMT.
As a key team member, has received the Zhejiang Provincial Science and Technology Progress First Prize and the National Science and Technology Progress Second Prize


