
Recently, the upper urinary tract reconstruction team led by Xuesong Li, Director of the Department of Urology at Peking University First Hospital, successfully performed a domestic surgical robot–assisted laparoscopic fully intracorporeal autologous kidney transplantation for a patient with complex upper urinary tract obstruction.The entire procedure was completed within the abdominal cavity and was characterized by minimal blood loss, reduced surgical trauma, and the elimination of extracorporeal kidney repair.

Professor Xuesong Li during surgery

Xuesong Li’s Surgical Team in the Operating Room
01
Benevolence with Integrity, Virtue as the Foundation
Mr. W, a 58-year-old man from Shandong Province, had experienced recurrent flank pain over the past three months. A CT scan performed at a local hospital revealed severe right hydronephrosis and a suspected mass in the right ureter. Subsequent ureteroscopic examination confirmed multiple polyps in the mid-ureter, and pathological findings indicated fibroepithelial polyps.
With a strong desire to preserve his kidney, Mr. W sought treatment at Peking University First Hospital. The urology team led by Xuesong Li promptly performed a percutaneous nephrostomy to relieve obstruction, ensure effective drainage, and preserve renal function.
Upper urinary tract imaging and contrast-enhanced CT with three-dimensional reconstruction demonstrated marked tortuosity and dilation of the middle and upper segments of the right ureter, accompanied by multiple annular strictures and extensive intraluminal filling defects, measuring approximately 7–8 cm in length.
Mr. W was diagnosed with a newly identified disease phenotype recently described by Xuesong Li’s team—MASTUMP syndrome, characterized by the triad of Multiple Annular Stenosis, Tortuous Ureter, and Multifocal Polyps. Surgical management of this condition is highly challenging, and conventional reconstructive approaches are often insufficient.

Preoperative antegrade and retrograde urography of the patient
Preoperative Contrast-Enhanced CT with Three-Dimensional Reconstruction
Based on the absence of a large postoperative pathological specimen, the fact that the ureteral lesions were mainly confined to the middle and upper segments, and that the distal ureteral lumen was normal, Xuesong Li proposed a more physiologically appropriate surgical strategy. After resection of the diseased middle and upper segments of the ureter, a fully intracorporeal autologous kidney transplantation was performed: the kidney was transplanted into the ipsilateral iliac fossa, and the renal pelvis was directly anastomosed to the distal ureter, thereby restoring normal ureteral physiological function.
After thorough discussion, the team concluded that autologous kidney transplantation avoids the need to use other tissues for reconstruction, thus reducing injury to additional organs. It also circumvents the metabolic complications associated with ileal ureter substitution, such as electrolyte disturbances caused by urine absorption, while lowering the risks of intestinal fistula and bowel obstruction. Furthermore, complete preservation of the intramural bladder segment prevents vesicoureteral reflux and urinary tract infection. This surgical approach enables restoration of normal urinary drainage postoperatively and significantly minimizes the impact on the patient’s quality of life.
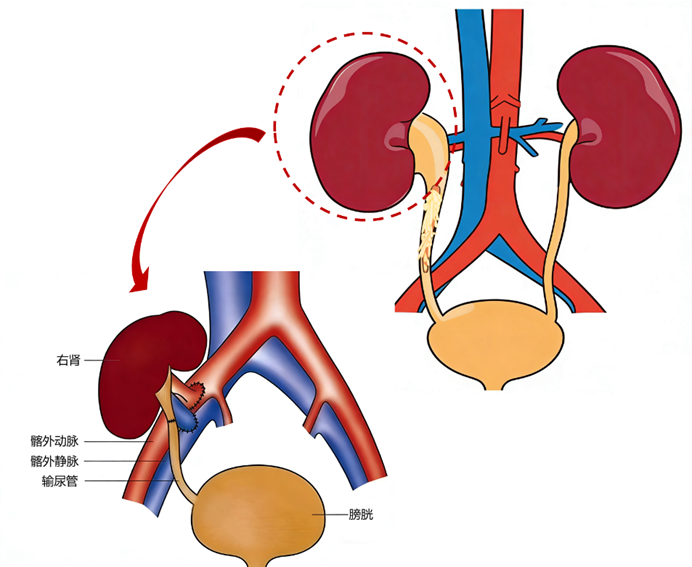
Surgical Plan Simulation Diagram
02
Upholding the Way Through Collaboration, Uniting Strength to Break Barriers
Standard robot-assisted laparoscopic autologous kidney transplantation typically involves robotic nephrectomy followed by open, extracorporeal kidney repair and subsequent transplantation. This approach still has limitations, including relatively greater surgical trauma and slower recovery. In contrast, fully intracorporeal robot-assisted autologous kidney transplantation represents the cutting edge of minimally invasive surgery and is currently performed at only a handful of major medical centers worldwide.
With domestic robotic systems now reaching technical maturity, an important question emerged: Can a domestically developed robot safely and effectively perform fully intracorporeal kidney transplantation? Building on prior experience with fully robotic autologous kidney transplantation, Xuesong Li, together with Caiyong Lai, Chief Physician of Urology at the Miyun Campus of Peking University First Hospital, collaborated closely with the anesthesia team and operating room nursing staff. The team meticulously designed the surgical plan as well as intraoperative and postoperative management protocols. Based on the patient’s anatomical features and disease characteristics, every surgical detail was carefully planned and repeatedly rehearsed in advance.
03
Synergy for Long-Term Success, Precision in Every Millimeter
In the operating room, Xuesong Li skillfully operated a new-generation domestically developed robotic surgical system. Leveraging a clear three-dimensional high-definition view and highly flexible robotic arms, the team achieved precise lesion resection and delicate anastomosis. Meanwhile, the anesthesia team and operating room nursing staff worked in seamless coordination, ensuring patient safety and the smooth execution of the procedure.

The Operating Room Team United to Complete a Highly Challenging Procedure
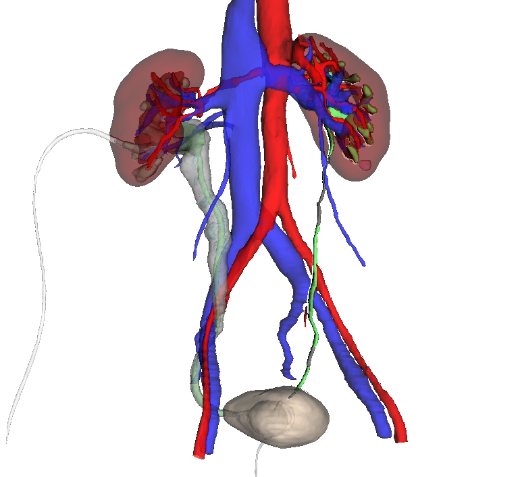
The surgery was performed in two stages. In the first stage, with the assistance of CT-based three-dimensional reconstruction and cognitive fusion imaging, the patient was placed in the lateral decubitus position. Precise dissection and mobilization of the affected kidney and the middle-to-upper segments of the ureter were completed. Using fluorescence guidance for accurate localization, the ureteral segment narrowed by multiple polyps was resected (as shown in the figure). After complete mobilization of the kidney, the renal artery and vein were transected, followed immediately by intracorporeal renal cold perfusion, limiting the warm ischemia time to 2 minutes and 8 seconds.
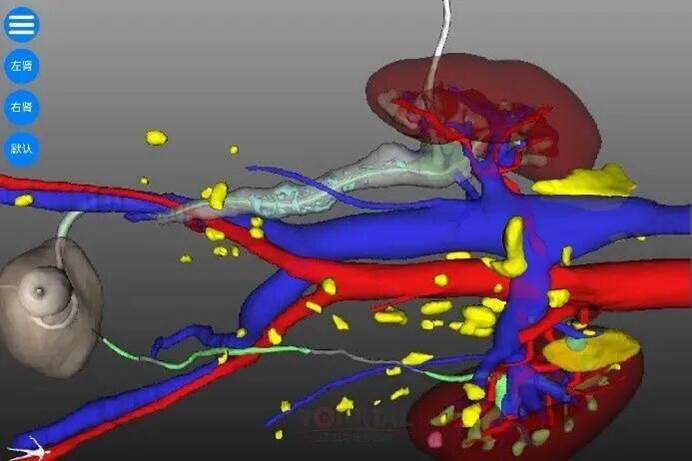
CT-based three-dimensional reconstruction and cognitive fusion technology assisting intraoperative decision-making
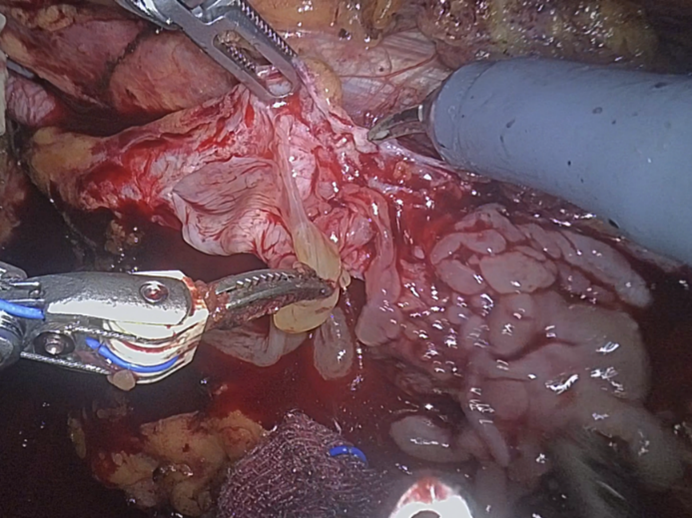
Intraoperative exploration and resection of the ureteral segment narrowed by polyps

Resected Polyp-Induced Stenotic Segment
In the second stage, while continuous intracorporeal cold perfusion at 0–4 °C was maintained to preserve the kidney, the patient was repositioned to a supine position with the head lowered and feet elevated. The robotic system was then re-docked to complete trimming of the renal vessels, followed by anastomosis of the renal artery and vein to the external iliac artery and vein, as well as ureteral anastomosis.
To ensure adequate perfusion temperature, the operating room nursing team closely monitored and managed the temperature of the perfusion solution, maintaining the kidney in an optimal cold ischemic state. With robotic assistance, the arterial and venous anastomoses were performed with high precision and reliability. After removal of the vascular clamps, blood flow to the kidney was rapidly restored, with the graft appearing well perfused and pink in color. Intraoperative Doppler ultrasonography confirmed good vascular patency of the transplanted kidney.

Patient repositioning and re-docking of the robotic system

After Restoration of Renal Blood Flow, the Kidney Appeared Well Perfused; Intraoperative Ultrasound Demonstrated Good Blood Flow Signals
Postoperatively, the patient recovered well, with stable renal function parameters. This high-intensity procedure, lasting five hours, vividly demonstrated the seamless integration of Xuesong Li’s superb surgical expertise, the team’s strong collaborative spirit, and the outstanding performance of the domestically developed Kangduo robotic surgical system.
04
Strength Built Over Time, Setting a New Benchmark
According to a preliminary review of the literature, this case represents the first reported fully intracorporeal robot-assisted autologous kidney transplantation in China, as well as the first such procedure worldwide performed using a domestically developed surgical robot. The operation not only establishes a new minimally invasive treatment paradigm for long-segment ureteral disease, but also reflects Peking University First Hospital’s enduring commitment to a patient-centered philosophy. At the same time, it underscores that true clinical innovation is born from rigorous collaboration and sets new benchmarks by upholding foundational principles while pursuing breakthrough advances.


