
On January 28, a landmark study was published in the world-leading medical journal The BMJ. For the first time, a multicenter randomized controlled trial (RCT) has demonstrated that the reliability of urological telesurgery is non-inferior to conventional local robotic surgery.The study, entitled “Reliability of Urological Telesurgery Compared to Local Surgery: A Multicenter, Randomised Controlled Trial,” was jointly conducted by five medical centers in China, providing critical scientific evidence for the large-scale clinical implementation of telesurgery.
The first author was Ye Wang, MD (Chinese PLA General Hospital).
Co–first authors included Dan Xia, MD (The First Affiliated Hospital, Zhejiang University School of Medicine), Mulat Reshat, MD (The First Affiliated Hospital of Xinjiang Medical University), and Wuyi Zhao, Engineer (Edge Medical Technology Co., Ltd., Shenzhen).
Corresponding authors were Xu Zhang, Academician (Chinese PLA General Hospital), Hongzhao Li, MD, Xin Ma, MD (Chinese PLA General Hospital), and Zhaochao Liang, MD (The First Affiliated Hospital of Anhui Medical University).

Study Background
Breaking the Geographic Barriers of Surgery
Traditional surgery has long been constrained by the requirement that surgeons and patients must be in the same physical location, making it difficult to meet urgent surgical needs in remote regions, disaster zones, military settings, or space missions.
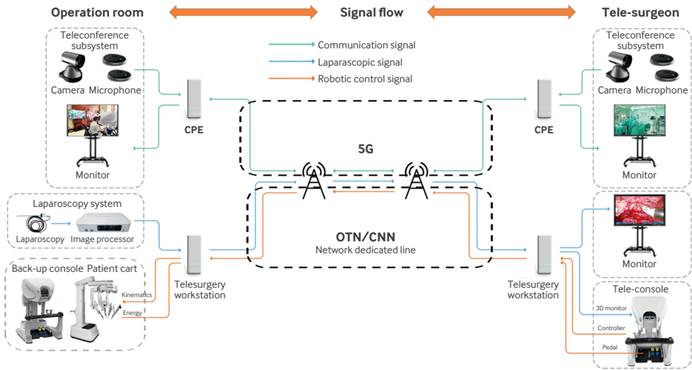
Telesurgery overcomes this limitation by integrating three core technologies:
- a surgeon console,
- a patient-side robotic system, and
- an ultra-low-latency communication network (e.g., dedicated optical fiber, 5G/6G wireless networks, or satellite communication).
This system enables surgeons to remotely and precisely control robotic instruments to perform surgery. Since the world’s first transatlantic telesurgical cholecystectomy in 2001, progress in telesurgery has been slow due to limitations in communication stability and robotic precision. However, recent advances in high-speed networking and domestically developed surgical robots have driven rapid progress in this field.
Study Design
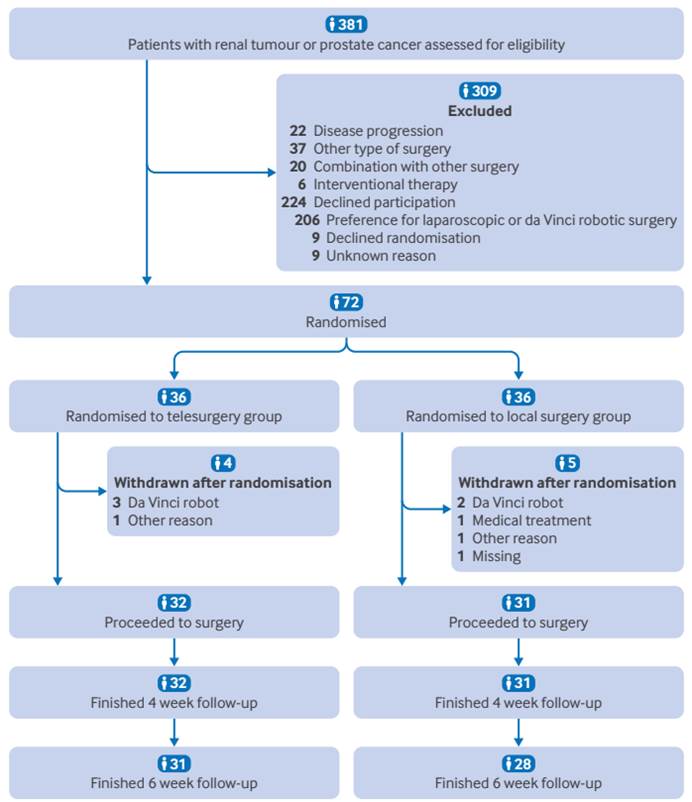
This study adopted a multicenter, non-inferiority, randomized controlled design. Between December 2023 and June 2024, a total of 72 patients scheduled for radical prostatectomy or partial nephrectomy were enrolled and randomly assigned (1:1) to either a telesurgery group or a local surgery group.
The predefined non-inferiority margin was an absolute difference in surgical success rate of 0.1 (i.e., telesurgery would be considered non-inferior if its success rate was no more than 10% lower than that of local surgery).
Telesurgical System Architecture
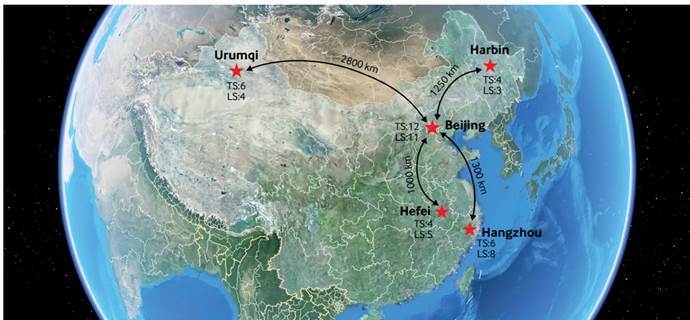
The telesurgery platform consisted of three major subsystems. The communication network covered four long-distance routes from Beijing to:
- Urumqi (2,800 km),
- Harbin (1,250 km),
- Hangzhou (1,300 km), and
- Hefei (1,000 km).
Dedicated Optical Transport Network (OTN) and Cloud Connection Network (CCN) lines were used to ensure stable and secure data transmission.
Study Results
100% Telesurgical Success Rate With Stable Technical Performance
1. Primary Endpoint: Non-Inferiority of Surgical Success Rate
In the intention-to-treat analysis, the surgical success rate was:
- 100% (36/36) in the telesurgery group, and
- 94.44% (34/36) in the local surgery group.
Bayesian mixed-effects logistic regression showed a success-rate difference of 0.02 (95% credible interval: −0.03 to 0.15). The posterior probability of non-inferiority was 0.99, well above the prespecified threshold of 0.975.
Only one surgical failure occurred, in the local surgery group, due to robotic system malfunction; the procedure was completed after switching to a backup system. No intraoperative conversion or serious complications occurred in the telesurgery group.
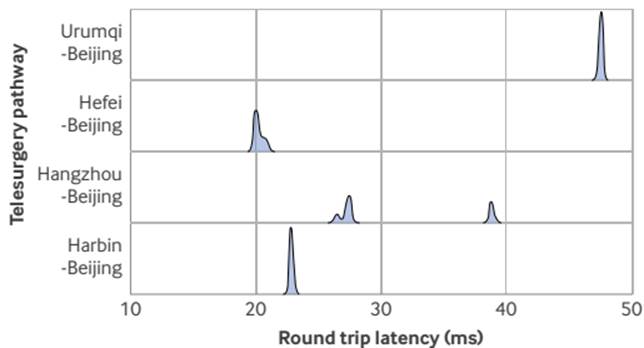
2. Technical Performance: Long-Distance Latency Remained Controllable
The telesurgery system remained stable across transmission distances ranging from 1,000 km to 2,800 km. Mean round-trip network latencies were:
- 47.5 ms (Urumqi–Beijing),
- 30.6 ms (Hangzhou–Beijing),
- 22.8 ms (Harbin–Beijing), and
- 20.1 ms (Hefei–Beijing).
Frame loss was minimal, averaging 0–1.5 frames per procedure, with no impact on surgical precision.
3. Clinical Outcomes: No Significant Differences Between Groups
Operative parameters:
Median operative time was 151.5 minutes in the telesurgery group and 135.0 minutes in the local group (adjusted mean difference: 13.67 minutes, P = 0.87). Intraoperative blood loss and warm ischemia time for partial nephrectomy did not differ significantly between groups.
Postoperative recovery:
Length of hospital stay, intensive care unit duration, complication rates (Clavien–Dindo classification), Quality of Recovery-15 (QoR-15) scores, and the 30-second sit-to-stand test were comparable between groups.
Oncologic outcomes:
The positive surgical margin rate was 3.1% (1/32) in the telesurgery group and 16.1% (5/32) in the local surgery group, a difference that warrants further validation in larger cohorts.
4. Surgical Team Workload: Reduced Burden for Primary Surgeons
Using the NASA Task Load Index, the workload score of the primary surgeon was significantly lower in the telesurgery group than in the local surgery group (29.0 vs 48.0, P = 0.004). No differences were observed for assistants or scrub nurses.
The authors noted that this finding may be influenced by the non-blinded study design, but it suggests that the telesurgical interface may help optimize workflow and ergonomics.
Clinical Significance
Promoting Equity in Healthcare Resource Distribution
China is a representative country with uneven distribution of high-quality medical resources, which are concentrated in major urban centers while remote regions remain underserved. Telesurgery has the potential to reduce the burden of cross-regional patient travel and to address increasing surgical demand driven by population aging and earlier onset of malignancies.
Previous exploratory studies by the research team had demonstrated the feasibility of telesurgery across various urologic procedures. This RCT provides the highest level of evidence to date, laying a solid foundation for larger-scale clinical trials and broader implementation.
Conclusion
This study marks a transition of telesurgery from technological exploration to evidence-based clinical validation. With continued advances in communication infrastructure and robotic systems, telesurgery is poised to reshape global healthcare delivery, allowing top-tier surgical expertise to transcend geographical and temporal boundaries and benefit a far wider patient population.


![[The Lancet] Professor Yungang Tao: Breaking Two Decades of Stagnation—The NIVOPOST-OP Trial Redefines Postoperative Adjuvant Therapy for High-Risk Head and Neck Squamous Cell Carcinoma](https://mediamedic.co/wp-content/uploads/2026/02/image-5-150x150.png)