With the rapid advancements in medical technology and deeper insights into the mechanisms of lymphoma, traditional chemotherapy is gradually giving way to a new era of precision-targeted and immunotherapies. Innovative drugs are emerging like bamboo shoots after the rain, offering personalized treatment paths tailored to lymphoma patients. This marks the dawn of a new era in disease management, with the promise of more effective and optimistic treatment outcomes. At the 12th Lu Daopei Hematology Forum, Hematology Frontier invited Dr. Hongmei Jing from Peking University Third Hospital to provide a comprehensive analysis of the current state of lymphoma treatment in China, explore future research directions, and discuss the field's ongoing development.Hematology Frontier: In recent years, significant progress has been made in lymphoma treatment. Could you highlight some of the emerging drugs or research outcomes that deserve our attention?
Dr. Hongmei Jing: Over the long history of lymphoma treatment, chemotherapy has dominated as the mainstream therapy for decades. However, with the rapid development of medical technology and a deeper understanding of disease mechanisms, treatment strategies for lymphoma are undergoing unprecedented changes, moving towards more precise, efficient, and less toxic approaches. The shift from traditional cytotoxic chemotherapy to targeted therapies focused on specific molecular targets has opened a new chapter in lymphoma treatment.
Starting with the introduction of CD20 monoclonal antibodies, a series of innovative drugs have emerged, including antibody-drug conjugates (ADCs) and bispecific antibodies. These drugs precisely target specific antigens on the surface of cancer cells, delivering selective cytotoxicity while minimizing harm to normal cells. Moreover, the introduction of immunomodulatory drugs has further refined the lymphoma treatment landscape. The widespread use of these therapies provides patients with richer, more personalized treatment options, further advancing the field of lymphoma therapy.
Notably, the development of inhibitors targeting the B-cell receptor signaling pathway, such as Bruton’s tyrosine kinase (BTK) inhibitors, has marked the beginning of a new era of precision-targeted therapy in lymphoma. Currently, four BTK inhibitors have been approved in China: ibrutinib, acalabrutinib, zanubrutinib, and orelabrutinib, each demonstrating excellent efficacy in specific indications.
In summary, the innovations and breakthroughs in lymphoma treatment not only reflect the rapid advancement of medical technology but also demonstrate humanity’s steadfast determination and tireless efforts to conquer this stubborn disease. As research into lymphoma mechanisms deepens and new therapeutic techniques emerge, we have every reason to believe that lymphoma patients will have more and better treatment options, heralding a brighter future for their health.
Hematology Frontier: In comprehensive lymphoma treatment, how do you balance chemotherapy, biological therapy, and other treatment modalities to achieve the best therapeutic outcomes?
Dr. Hongmei Jing: When treating newly diagnosed lymphoma patients, an individualized and precise treatment strategy is recommended, with treatment plans tailored to each patient’s unique clinical background and disease status. First, a comprehensive assessment of the patient’s overall condition is essential, including factors such as age, physical status, comorbidities, and underlying diseases, to determine their treatment tolerance. This process is crucial, as it directly influences the formulation and execution of the subsequent treatment plan.
For elderly patients, especially those over 80, their physiological function may be declining, and they are often less tolerant of intensive treatment. In such cases, a gentler “light chemotherapy” approach is favored. This involves reducing the dosage and frequency of chemotherapy drugs to minimize treatment-related toxicity, while actively exploring and prioritizing new therapies such as immunotherapy and small molecule targeted drugs. These treatments can effectively control the disease while reducing the burden on patients, achieving the concept of light or even chemotherapy-free treatment.
On the other hand, for younger and physically fit patients with rapidly progressing disease, a more aggressive treatment strategy may be adopted. In such cases, chemotherapy can be combined with emerging drugs, such as immune checkpoint inhibitors, to enhance treatment efficacy through multi-targeted, multi-modal action. This approach increases the possibility of achieving long-term disease control and even cure.
Therefore, a personalized treatment model based on precision medicine principles strives to ensure patient safety while achieving the best possible therapeutic outcomes, enabling every patient to benefit from medical advancements.
Hematology Frontier: Could you share some challenges you have encountered in lymphoma treatment and your strategies for addressing them? What key issues do you believe future research should focus on?
Dr. Hongmei Jing: Two main challenges stand out in the field of lymphoma treatment. The first core issue is the challenge of relapse in aggressive lymphomas. These lymphomas are characterized by their highly aggressive nature and potential chemotherapy resistance. Some patients may experience early relapse despite initial treatment. In such cases, subsequent treatment strategies need to shift to more innovative and differentiated approaches to provide greater therapeutic benefits. When first- and second-line chemotherapy regimens show resistance or poor efficacy, it is recommended to explore emerging therapies, such as antibody-drug conjugates (ADCs) and chimeric antigen receptor T-cell (CAR-T) therapies, to achieve rapid and profound disease control, potentially extending progression-free survival (PFS) and offering the possibility of a cure.
The second challenge lies in treating indolent lymphomas, which are characterized by slow progression but a high relapse rate, making complete cure difficult. In this context, the focus is on deepening remission and extending PFS. To achieve this goal, the medical community is actively exploring the integration of emerging drugs into classical treatment regimens to optimize therapeutic outcomes and delay disease progression.
Overall, individualized and precision treatment strategies have become the consensus in addressing the challenges of lymphoma treatment. By combining traditional therapies with emerging treatments and continuously optimizing treatment regimens, we aim to provide patients with safer, more effective, and personalized treatment options, ultimately improving lymphoma treatment outcomes.
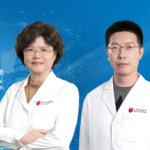
Dr. Hongmei Jing
Director of the Hematology Department, Peking University Third Hospital Professor, Chief Physician, Ph.D. Supervisor
Positions held:
- Vice Chairperson, Oncology Expert Committee, Chinese Medical Women’s Association
- Vice Chairperson, Lymphoma Committee, China Medical Education Association
- Vice Chairperson, Hematology Committee Youth Group, China Medical Education Association
- Chairperson, Hematologic Oncology Committee, Beijing Integrative Medicine Society
- Standing Committee Member, Geriatric Oncology Committee, Chinese Society of Geriatrics
- Committee Member, Diagnostic Group, Chinese Society of Hematology
- Committee Member, Hematology Branch, Chinese Medical Doctor Association
Professor Jing has presided over and participated in numerous research projects funded by the National Natural Science Foundation of China, Beijing Natural Science Foundation, and “985 Multi-Center Research” at Peking University Medical School, among others.
She has received the Second Prize for Scientific and Technological Progress from the Higher Education Research Excellence Awards and has published more than 60 papers and contributed to 5 books.