
In 2023, a groundbreaking study spearheaded by Professor XiaoJun Huang from Peking University Institute of Hematology, made its debut in a prestigious international academic journal——Bone Marrow Transplantation. This pivotal research, entitled “Comparison of Haploidentical Hematopoietic Stem Cell Transplantation with Chemotherapy in Older Adults with Acute Myeloid Leukemia” offers a novel perspective on treatment efficacy for Acute Myeloid Leukemia (AML) in the elderly population. The study meticulously explores the viability and outcomes of using haploidentical donors for stem cell transplantation compared to traditional chemotherapy approaches, marking a significant advancement in the therapeutic landscape for older AML patients.
Acute myeloid leukemia (AML) is a formidable challenge in oncology, particularly in the older population. The standard treatment options, primarily consisting of chemotherapy and allogeneic hematopoietic stem cell transplantation (allo-HSCT), have limited effectiveness in this age group due to higher morbidity and mortality rates. The advent of haploidentical stem cell transplantation (haplo-SCT) presents a new therapeutic avenue. This approach leverages stem cells from partially matched family donors, thereby vastly expanding the donor pool beyond matched sibling donors (MSD) and unrelated donors (URD), who are often scarce for many patients. Despite the theoretical advantages, the comparative effectiveness and safety of haplo-SCT versus conventional chemotherapy in older AML patients remain underexplored.
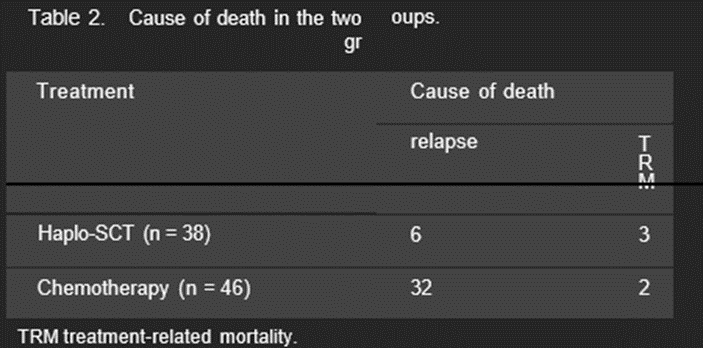
The study in question adopted a retrospective design to compare outcomes between older AML patients undergoing haplo-SCT and those receiving consolidation chemotherapy after achieving the first complete remission (CR1). This comparison was grounded in several inclusion criteria: age between 55 and 65 years, a diagnosis of intermediate or high-risk AML, and achievement of CR1 following no more than two cycles of induction therapy. The analysis encompassed 46 patients in the chemotherapy cohort and 38 in the haplo-SCT group. This approach allowed for a nuanced examination of survival outcomes, relapse rates, and treatment-related mortality (TRM) across these distinct therapeutic strategies.
The comparison yielded compelling findings. Patients who underwent haplo-SCT demonstrated significantly improved overall survival (OS) and leukemia-free survival (LFS), alongside reduced relapse incidence, compared to those who received chemotherapy. Notably, the TRM rates did not differ significantly between the two groups, challenging the prevailing assumption that haplo-SCT inherently carries a higher risk of mortality in older patients. These results underscore haplo-SCT’s potential as a viable post-remission therapy for older adults with intermediate to high-risk AML, marking a significant departure from traditional reliance on chemotherapy alone.
AML acute myeloid leukemia, G-CSF granulocyte colony-stimulating factor, HMAs hypomethylating agents, CR complete remission, BM bone marrow, PB peripheral blood.

The study’s findings suggest a paradigm shift in treating older AML patients, advocating for the consideration of haplo-SCT as a feasible alternative to consolidation chemotherapy. This recommendation is particularly pertinent for patients without access to matched donors, a common dilemma in this demographic. The improved survival outcomes associated with haplo-SCT highlight the technique’s evolution and its growing role in extending life expectancy and quality for older AML patients.
Nonetheless, the decision to pursue haplo-SCT must be carefully weighed against various factors, including disease characteristics, patient performance status, transplantation risks, and financial implications. The study also calls for further research to consolidate these findings, particularly through prospective trials that could offer more definitive evidence of haplo-SCT’s efficacy and safety in this patient population.
In conclusion, the advancement of haplo-SCT represents a promising development in the fight against AML in older adults. As our understanding of this modality deepens, it holds the potential to significantly alter treatment landscapes and improve outcomes for a demographic historically plagued by limited therapeutic options and poor prognoses.


