
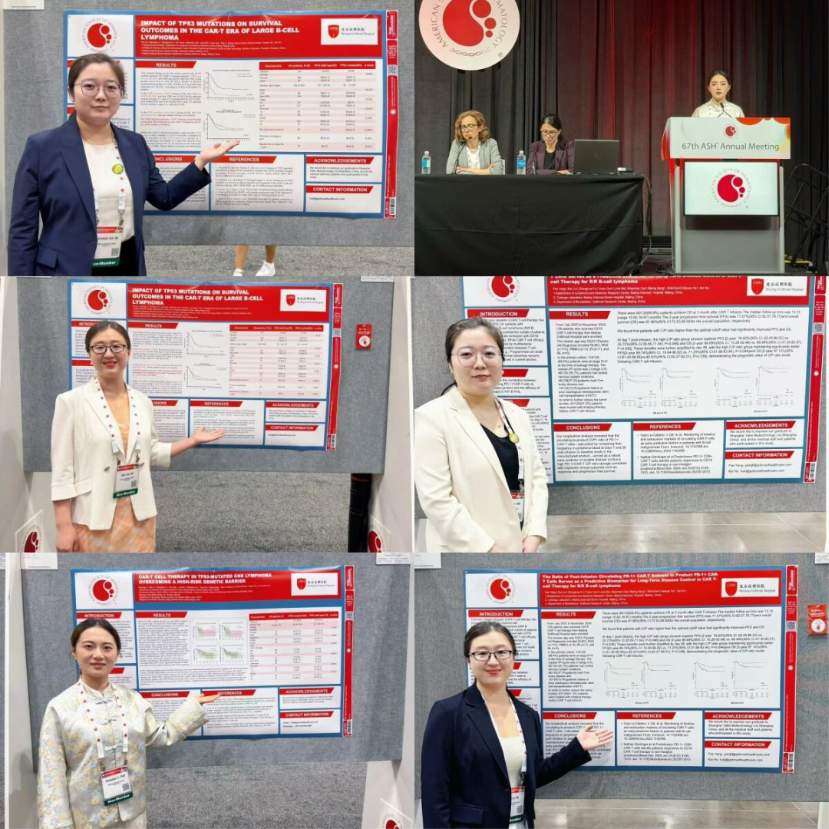
The 67th Annual Meeting of the American Society of Hematology (ASH) was held from December 6 to 9, 2025, in Orlando, bringing together the latest global advances in hematology research and clinical practice. At this year’s meeting, the team led by Professor Hu Kai from Beijing Gaobo Hospital presented seven studies focusing on CAR-T cell therapy across different types of relapsed/refractory lymphoma, including B-cell lymphoma, central nervous system lymphoma, T-cell lymphoma, as well as combined strategies involving CAR-T therapy and hematopoietic stem cell transplantation. These studies provide important evidence supporting the further development of individualized treatment strategies. Oncology Frontier – Hematology Frontier invited Professor Hu Kai to provide an in-depth interpretation of these key findings and their clinical significance. Oncology Frontier – Hematology Frontier
At this year’s ASH meeting, your team presented several studies. Could you first provide an overall overview? What clinical pain points do these studies aim to address?
Professor Hu Kai: At this year’s ASH Annual Meeting, our team presented a total of seven research studies. These projects were developed based on the clinical strengths of our department and focused on relapsed/refractory lymphoma and multiple myeloma, with a particular emphasis on cellular immunotherapy, especially innovative applications of CAR-T cell therapy.
First, we reported data from two prospective phase I clinical trials. One evaluated the efficacy of CD19 CAR-T therapy in relapsed/refractory central nervous system lymphoma, while the other assessed the efficacy and long-term outcomes of CD7 CAR-T therapy in T lymphoblastic leukemia/lymphoma.
Second, we explored salvage strategies using hematopoietic stem cell transplantation in patients who failed CD19 CAR-T therapy. Although CD19 CAR-T therapy has become one of the most effective treatments for relapsed/refractory lymphoma, a subset of patients still experiences disease progression. Stem cell transplantation may offer these patients another opportunity for remission or even long-term cure. In this study, we compared outcomes between autologous and allogeneic transplantation cohorts.
In addition, we conducted biomarker studies aimed at predicting CAR-T treatment efficacy, focusing on TP53 mutations in tumor cells and the dynamic changes in PD-1 expression and exhaustion status of CAR-T cells in vivo. These biomarkers may help predict treatment response and support more precise therapeutic decision-making in the future.
Oncology Frontier – Hematology Frontier
Based on your team’s findings, could you systematically explain recent breakthroughs in efficacy prediction and prognostic improvement of CAR-T therapy among molecularly high-risk B-cell lymphoma patients? How do these findings inform clinical decision-making?
Professor Hu Kai: One of our major research focuses this year was identifying clinically meaningful predictive biomarkers for CAR-T therapy in B-cell lymphoma. This stems from a very real clinical need: patients and their families are eager to understand the likelihood of benefit from CAR-T therapy in individual disease contexts.
Our data revealed two key findings. The first relates to TP53 mutations, which have long been recognized as adverse prognostic factors in the chemotherapy era, significantly reducing the efficacy of chemotherapy and autologous stem cell transplantation in both CNS lymphoma and diffuse large B-cell lymphoma. In the CAR-T era, our study demonstrated that although TP53 mutations still exert a negative influence, CAR-T therapy can partially overcome this adverse effect, leading to improved treatment responses and long-term survival compared with conventional therapies.
The second finding involves the dynamic exhaustion status of T cells. We observed that changes in PD-1 expression from pre-infusion to post-infusion, particularly a transition from low to high PD-1 expression, were associated with enhanced CAR-T activation and better clinical outcomes. This dynamic biomarker not only aids in efficacy prediction but also provides a rationale for future strategies combining CAR-T therapy with PD-1 blockade to optimize treatment outcomes.
Overall, as CAR-T therapy continues to mature, its management is expected to evolve from purely clinical refinement toward precision-driven, biomarker-guided, and data-informed approaches.
Oncology Frontier – Hematology Frontier
Central nervous system lymphoma has long had limited treatment options. Based on the studies presented at ASH, could you discuss the latest progress of CAR-T therapy in relapsed/refractory CNS lymphoma and the key factors influencing efficacy?
Professor Hu Kai: This year, our team conducted two studies in the field of CNS lymphoma, one of which was a prospective phase I clinical trial evaluating CD19 CAR-T therapy in relapsed/refractory CNS lymphoma. While real-world data have suggested potential efficacy, prospective evidence had been lacking. Our study addressed this gap and was selected for oral presentation at ASH.
The results demonstrated that CD19 CAR-T therapy is effective in this patient population. We also identified several factors influencing efficacy, including patient age, disease stage, and response to tumor debulking therapy prior to CAR-T infusion. Notably, adequate disease control before CAR-T therapy emerged as a key determinant of subsequent treatment success.
In summary, CAR-T therapy represents a highly promising option for CNS lymphoma. Future prospective studies and combination strategies will be essential to identify the patients most likely to benefit and to further enhance treatment outcomes.
Oncology Frontier – Hematology Frontier
T-cell lymphoma is considered one of the most challenging areas for CAR-T therapy. Could you introduce the innovative aspects of your CD7 CAR-T study and its implications for improving long-term outcomes?
Professor Hu Kai: T-cell lymphoma has become a frontier area in CAR-T research. Although short-term responses have been encouraging, long-term outcomes remain inferior compared with B-cell lymphomas. At this ASH meeting, we reported phase I clinical data on CD7 CAR-T therapy in T-cell lymphoma.
Compared with previous studies, our research expanded the treated population to include not only T lymphoblastic leukemia/lymphoma but also mature T-cell lymphomas, broadening the potential applicability of CD7 CAR-T therapy.
We also employed a low-dose CAR-T infusion strategy. Despite the reduced dose, the overall response rate exceeded 80%, indicating that robust antitumor activity can be achieved without high-dose infusion.
Importantly, long-term follow-up showed that patients achieving durable remission or cure were predominantly those who proceeded to allogeneic hematopoietic stem cell transplantation after CAR-T therapy. This suggests that CD7 CAR-T therapy should be viewed as a bridge to transplantation in eligible patients to maximize long-term benefit.
Oncology Frontier – Hematology Frontier
With the continuous evolution of CAR-T therapy, combined strategies involving transplantation have gained attention. Could you share your perspective on the clinical value, patient selection, and future directions of CAR-T plus transplantation?
Professor Hu Kai: Currently, combining CAR-T therapy with autologous stem cell transplantation has become an important strategy for relapsed/refractory lymphoma. This year, we focused on patients who failed CD19 CAR-T therapy, a particularly challenging “double-refractory” population.
Our findings indicate that if such patients respond to tumor debulking regimens, including targeted therapies, subsequent consolidation with autologous transplantation plus alternative CAR-T approaches or allogeneic transplantation combined with donor-derived CAR-T therapy can achieve meaningful clinical benefit.
These results highlight the importance of understanding the complementary mechanisms of CAR-T therapy and transplantation, as well as the need for precise patient selection to ensure that those most likely to benefit receive these intensive combination strategies. Overall, our work provides valuable clinical evidence to guide individualized and precision-based treatment planning for relapsed/refractory lymphoma.
Appendix: Overview of Professor Hu Kai’s Team Presentations at ASH 2025
Prospective and translational studies presented at ASH 2025 by Professor Hu Kai’s team encompassed CAR-T therapy in CNS lymphoma, high-risk genetic subgroups, T-cell lymphoma, post–CAR-T transplantation strategies, genomic heterogeneity, and immune exhaustion biomarkers, reflecting comprehensive exploration across efficacy, safety, and precision medicine dimensions.
Expert Profile

Professor Hu Kai Beijing Gaobo Hospital
Professor Hu Kai is Director of the Lymphoma and Myeloma Department at Beijing Gaobo Hospital. With over 20 years of experience in hematologic malignancies, his clinical and research focus includes leukemia, lymphoma, and multiple myeloma, with particular expertise in CAR-T therapy, cellular immunotherapy, and stem cell transplantation. He is among the early pioneers of CAR-T therapy in China and has led or participated in more than 100 clinical studies, with extensive presentations at major international hematology conferences.


