Editor's Note: The 60th Annual Meeting of the American Society of Clinical Oncology (ASCO) was grandly held in Chicago, USA, from May 31 to June 4, 2024. As a premier global event, ASCO gathers oncology experts from around the world to discuss the latest advancements and future trends in the field. At this year's ASCO conference, several studies led by Professor Pei Dong from the Sun Yat-sen University Cancer Prevention and Treatment Center were selected, making a significant impact on the international stage. These studies not only represent new progress in the field of urologic oncology in China but also contribute to the global development of urologic oncology. "Oncology Frontier" has summarized these studies for our readers.
Abstract No: e16514
Real-world outcomes among patients with advanced/metastatic renal cell carcinoma (mRCC) treated with tyrosine kinase inhibitors (TKIs) monotherapy or TKI-IO combination therapy
First Author: Pei Dong
Background:
Tyrosine kinase inhibitors (TKIs) as monotherapy or in combination with immunotherapy (TKI-IO) are the standard first-line treatment for advanced renal cell carcinoma (RCC) both domestically and internationally.
Methods:
This retrospective study analyzed real-world survival data of 325 patients with advanced renal cell carcinoma who were enrolled and followed up at the Sun Yat-sen University Cancer Prevention and Treatment Center from January 1, 2015, to November 30, 2022. The median follow-up period was 26.1 months (range: 0-87.6). Real-world first-line progression-free survival (1L-rwPFS), real-world second-line progression-free survival (2L-rwPFS), and PFS2 (1L-rwPFS + 2L-rwPFS) were defined as the progression-free survival from the start of first-line treatment to the second-line progression.
Results:
A total of 325 patients were included, with a median age of 55 years (range: 16-83 years), 75% male (244 cases), and 25% female (81 cases). In cohort 1, 264 patients received 1L TKI monotherapy, while 61 patients in cohort 2 received 1L TKI-IO combination therapy. The median 1L-rwPFS for cohort 1 was 7.7 months, compared to 17.2 months for cohort 2 (HR 0.43, 95% CI: 0.32-0.56, P<0.00001). Sunitinib was the most commonly used TKI monotherapy, while axitinib combined with tislelizumab was the most frequent TKI-IO combination. The median PFS2 was longer for TKI-IO (32.6 vs. 24.8 months) (HR 0.42, 95% CI: 0.27-0.66, P<0.00001). In cohort 1, 37 patients chose second-line TKI monotherapy, while 211 patients received TKI-IO, with 2L TKI-IO having a longer 2L-rwPFS (14.2 vs. 7.5 months; HR 0.52, 95% CI: 0.33-0.83, P=0.00043). Similar trends were observed for PFS2 (20.3 vs. 27 months; HR 0.62, 95% CI: 0.40-0.96, P=0.0095). In the 211 patients of the 2L TKI-IO cohort, axitinib combined with IO was the most common regimen (182/211), with median 2L-rwPFS of 15.2 months for axitinib + IO and 8.2 months for other TKI + IO combinations (HR 0.41, 95% CI: 0.23-0.72, P<0.00001).
Conclusion:
Real-world data suggest that combination therapy is more effective than monotherapy in both first-line and subsequent lines of treatment, providing further evidence for the standard use of targeted immunotherapy for advanced renal cell carcinoma. Additionally, axitinib is the most commonly combined TKI in these therapies.
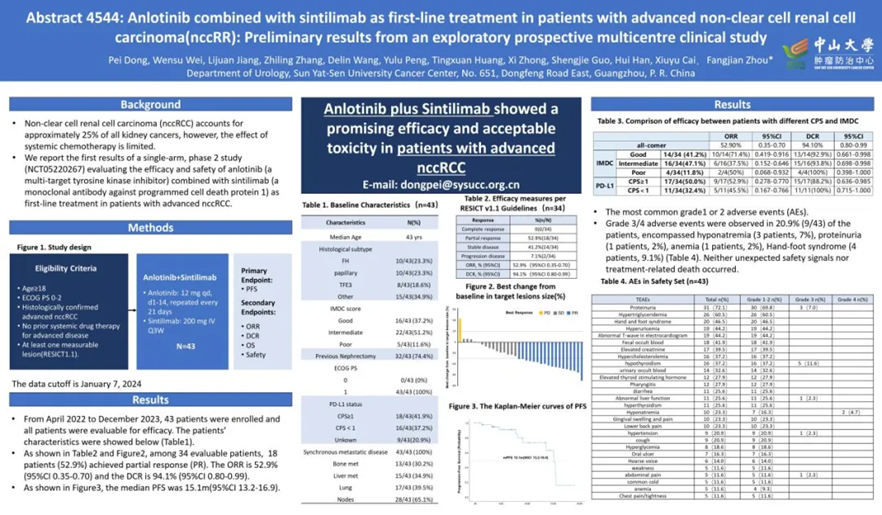
Abstract No: 4544
Anlotinib combined with sintilimab as first-line treatment in patients with advanced non-clear cell renal cell carcinoma (nccRCC): Preliminary results from an exploratory prospective multicenter clinical study
First Author: Pei Dong
Background:
Non-clear cell renal cell carcinoma (nccRCC) accounts for approximately 25% of all renal cancers, but systemic treatments are limited. We report the results of a single-arm phase II study (NCT05220267) to evaluate the efficacy and safety of anlotinib combined with sintilimab as first-line treatment for patients with advanced nccRCC.
Methods:
Patients included were ≥18 years old with an ECOG PS score of 0-2, pathologically confirmed nccRCC, no prior systemic therapy, and at least one measurable lesion (RECIST 1.1). Treatment included anlotinib (12 mg/day, 2 weeks on, 1 week off, 21-day cycles) and sintilimab (20 mg IV Q3W). The primary endpoint was progression-free survival (PFS), with secondary endpoints including objective response rate (ORR), disease control rate (DCR), overall survival (OS), and safety.
Results:
From April 2022 to December 2023, 43 patients were enrolled and evaluated. Among 34 evaluable patients, 18 (52.9%) achieved partial response (PR). The ORR was 52.9% (95% CI: 0.35-0.70) and DCR was 94.1% (95% CI: 0.80-0.99). The median PFS was 15.1 months (95% CI: 13.2-16.9). The most common adverse events (AEs) were grade 1 or 2. In 20.9% (9/43) of patients, grade 3/4 AEs were observed, including hyponatremia (3 cases, 7%), proteinuria (1 case, 2%), anemia (1 case, 2%), and hand-foot syndrome (4 cases, 9.1%). No unexpected safety signals or treatment-related deaths were observed.
Conclusion:
Anlotinib combined with sintilimab showed promising efficacy and acceptable toxicity in patients with advanced nccRCC.