Editor’s Note: Acute-on-chronic liver failure (ACLF) refers to a syndrome where, on the basis of chronic liver disease, the patient experiences a rapid deterioration of liver function within a short period, leading to acute or subacute hepatic decompensation. This presents as fatigue, jaundice, severe gastrointestinal symptoms, coagulation dysfunction, and other signs of liver failure. Currently, there is a lack of effective medical treatments, and the mortality rate is extremely high. Infections can induce or exacerbate ACLF and are one of the most common complications. According to related studies, the in-hospital mortality rate for ACLF patients with bacterial infections increases by 4-5 times. Therefore, the rapid identification of ACLF patients with concurrent infections and the prompt initiation of targeted anti-infection treatments are crucial for the disease progression and prognosis of ACLF patients. During the 32nd annual conference of the Asian Pacific Association for the Study of the Liver (APASL) in 2023, Professor Ning Qin from Tongji Hospital of Tongji Medical College, Huazhong University of Science and Technology, China, shared her group’s research progress.
Epidemiology of ACLF with Infection
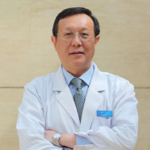
The types of infections associated with ACLF mainly include abdominal infections, urinary tract infections, respiratory infections, and skin and soft tissue infections. Localized infections can develop into bloodstream infections. The pathogens primarily involve Gram-negative bacteria (such as Klebsiella pneumoniae, Escherichia coli, Pseudomonas aeruginosa, etc.), Gram-positive bacteria (such as Enterococcus, Staphylococcus aureus, etc.), and in some cases, fungal infections like Candida (Figure 1).
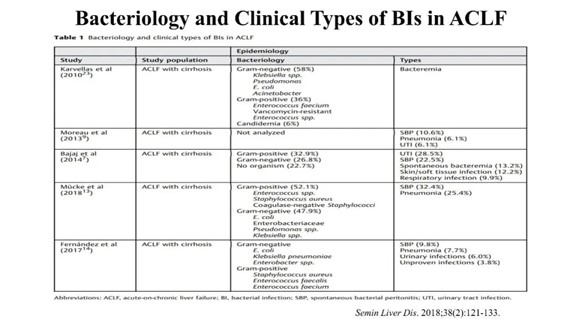
Figure 1. Common Pathogens and Clinical Types in ACLF Combined with Infection
Diagnosis of ACLF with Infection
Given that bacterial infection is one of the most common complications of ACLF, which can trigger or exacerbate conditions like variceal bleeding and hepatic encephalopathy, early and rapid diagnosis of bacterial infection can significantly reduce the mortality rate of ACLF. Numerous studies have focused on the early rapid diagnostic models for ACLF combined with infection. Since systemic inflammatory response plays a vital role in the development of ACLF with bacterial infection, using inflammatory markers as rapid diagnostic tools enables clinicians to make prompt and straightforward judgments with minimal clinical test results. For instance, a CRP level greater than 24.7 ng/mL as a threshold has a predictive area under the ROC curve of 0.811 for sepsis in patients with cirrhosis; a PCT level greater than 0.49 as a threshold has a predictive area under the ROC curve of 0.89. While the predictive efficacy of a single marker for infection is still limited, the combined use of CRP and PCT has greater diagnostic value (Figure 2). IL-6 can also be used as a biomarker for the early diagnosis of bacterial sepsis, and direct measurement of serum IL-6 levels can aid in the rapid diagnosis of bacterial infections, thereby preparing for subsequent treatment (Figure 3).
Figure 2. CRP and PCT as Tools for Early Diagnosis of Bacterial Infections
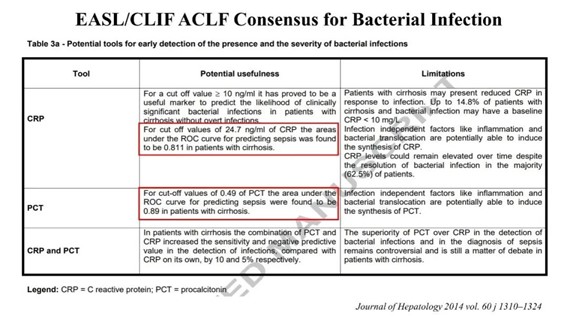
Figure 3. IL-6 as a Tool for Early Diagnosis of Bacterial Infections
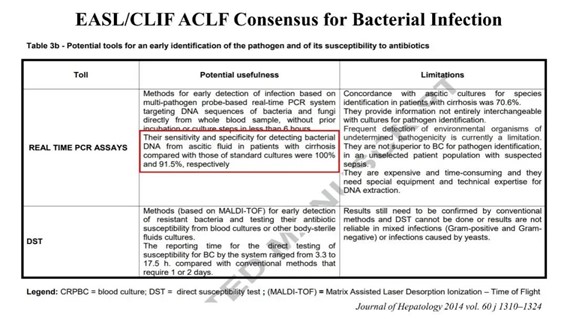
Additionally, the extraction of DNA from ascitic fluid for real-time fluorescent quantitative PCR analysis has shown high sensitivity and specificity, with rates of 100% and 91.5% respectively. However, due to limitations in equipment, technology, and economic conditions, this method has not yet been widely applied in clinical settings (Figure 4).
Figure 4. Tools for Early Diagnosis of Bacterial Infections
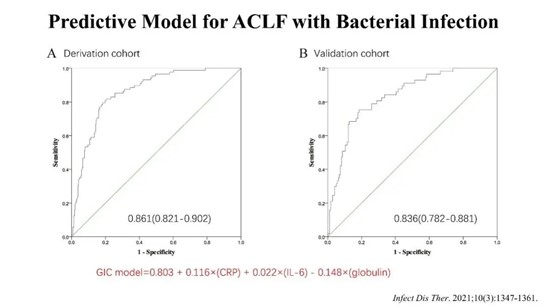
The aforementioned studies are primarily focused on the early diagnosis of bacterial infections, and currently, there is a lack of a clear predictive model. This research, based on a cohort of patients with HBV-related ACLF from the Infectious Disease Department of Tongji Hospital affiliated with Tongji Medical College, Huazhong University of Science and Technology, has established for the first time a predictive model for bacterial infections in patients with HBV-related ACLF. This model has been validated in a separate cohort and has shown good predictive value for the occurrence of infections in patients with HBV-related ACLF (Figures 5 and 6).
Figure 5. Predictive Model for Bacterial Infections in Patients with HBV-related ACLF
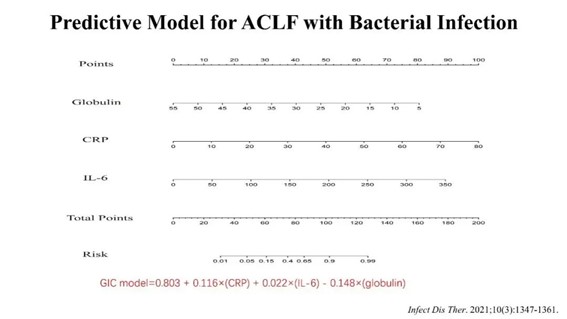
This figure likely presents the predictive model developed for identifying bacterial infections in patients suffering from acute-on-chronic liver failure (ACLF) related to Hepatitis B Virus (HBV). The model might include various clinical parameters, laboratory findings, and possibly imaging results that have been identified as significant predictors for bacterial infections in this specific patient group. The figure could feature statistical analyses, such as logistic regression outputs, ROC curves, or other relevant data visualization tools, which demonstrate the accuracy and reliability of the model in predicting bacterial infections in HBV-related ACLF patients.
Figure 6. ROC Curves of the Bacterial Infection Predictive Model in the Derivation and Validation Cohorts
Antimicrobial Treatment for ACLF Combined with Infection
Early and appropriate antibiotic treatment effectively improves patient prognosis and reduces mortality (Figure 7). Delaying the use of antibiotics offers no benefit to patient survival (Figure 8). Before obtaining pathogen identification and antibiotic susceptibility test results, the likely pathogens can be inferred based on the patient’s site of infection, clinical presentation, source of infection (hospital-acquired or community-acquired), past history of antimicrobial use and response to treatment. Combining this information with local bacterial resistance monitoring data, empirical antimicrobial therapy can be initiated (Figures 9-11).
Figure 7. Initiating Appropriate Antibiotic Therapy Within 24 Hours Benefits Survival in Patients with Cirrhosis Complicated by Bloodstream Infections
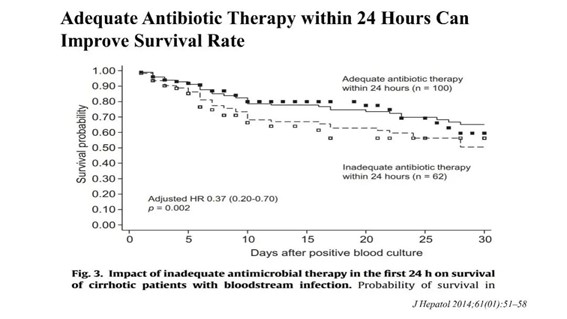
Figure 8. Delay in Antibiotic Use Increases Mortality Rate in Patients with Septic Shock

Figure 9. Recommendations for Empirical Antibiotic Treatment in Patients with Cirrhosis
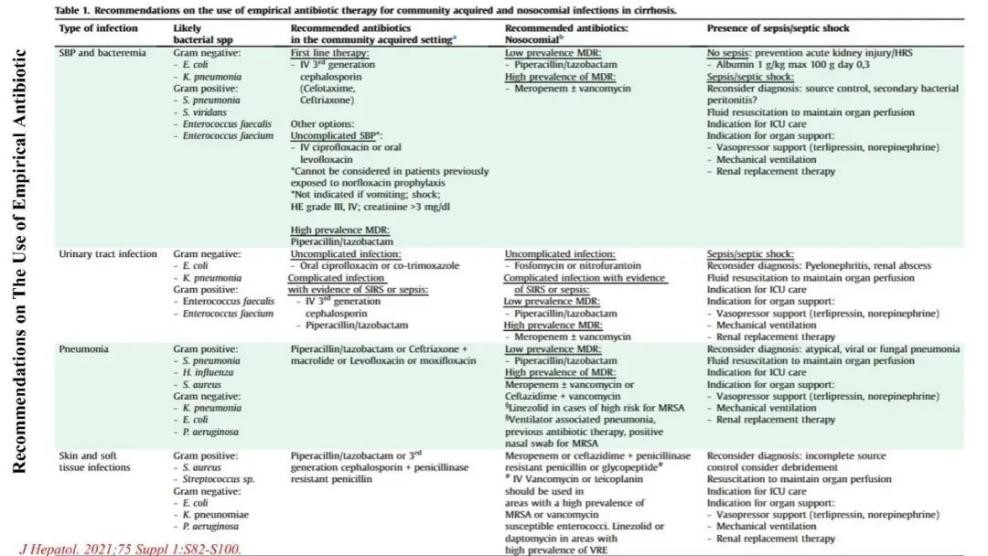
Figure 10. Recommendations for Empirical Antibiotic Treatment Regimens
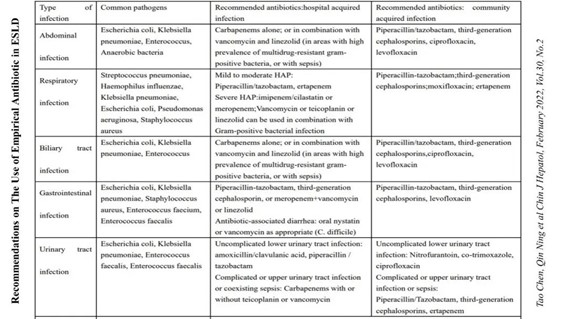
Figure 11. Recommendations for Empirical Antibiotic Treatment Regimens
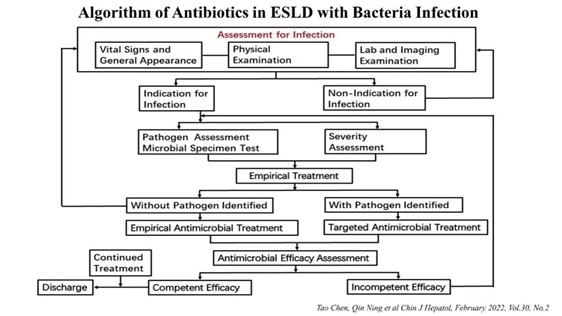
Before initiating empirical anti-infection treatment, qualified microbiological samples should be sent for pathogen examination. Once etiological evidence is obtained, the empirical anti-infection treatment should be promptly converted to targeted anti-infection treatment (Figures 12 and 13).
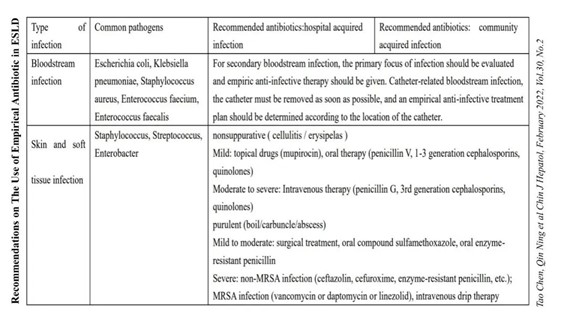
Figure 12. Expert Consensus on the Diagnosis and Treatment of End-Stage Liver Disease with Infection (2021 Edition)

Figure 13. Schematic Diagram of Antibiotic Use for End-Stage Liver Disease with Infection
Impact of Infection on Transplantation in ACLF
Liver transplantation is the only effective treatment for end-stage liver disease, and it should be considered when the patient’s life is severely threatened and medical treatment is ineffective. Besides the limitations posed by organ availability and economic factors, multiple studies have shown that the occurrence of infections adversely affects the long-term survival of liver transplant patients. Patients with uncontrolled infections are considered to have an absolute contraindication for liver transplant surgery (Figure 14). Preoperative aggressive anti-infection treatment does not negatively impact patient prognosis (Figures 15 and 16).
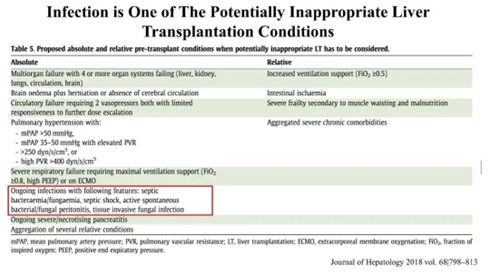
Figure 14. Persistent Infection as an Absolute Contraindication for Liver Transplant Surgery

Figure 15. Preoperative Aggressive Anti-infection Treatment Does Not Affect 30-Day Mortality Rate in Patients
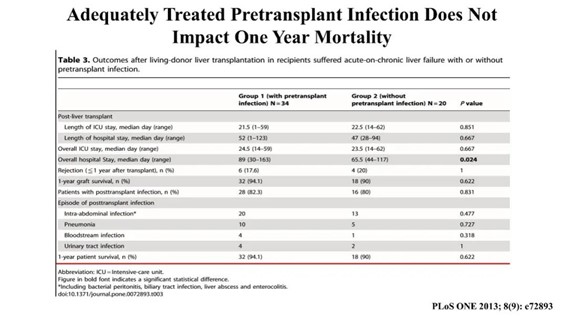
Figure 16. Preoperative Aggressive Anti-infection Treatment Does Not Affect One-Year Mortality Rate in Patients
ACLF often coincides with bacterial infections, typically leading to high mortality rates. Several diagnostic and predictive models have been developed for clinical reference. When ACLF patients have concurrent infections, it’s crucial to initiate empirical antibiotic treatment as soon as possible after confirming the pathogen with qualified samples. During treatment, careful attention should be paid to the patient’s drug resistance profile to minimize the development of multidrug-resistant bacteria. For patients anticipated to undergo liver transplantation, their infection status demands particular attention, as infections can adversely affect surgical outcomes. Timely and comprehensive treatment is essential in these cases.
TAG: APASL 2023, Voice of China, ACLF