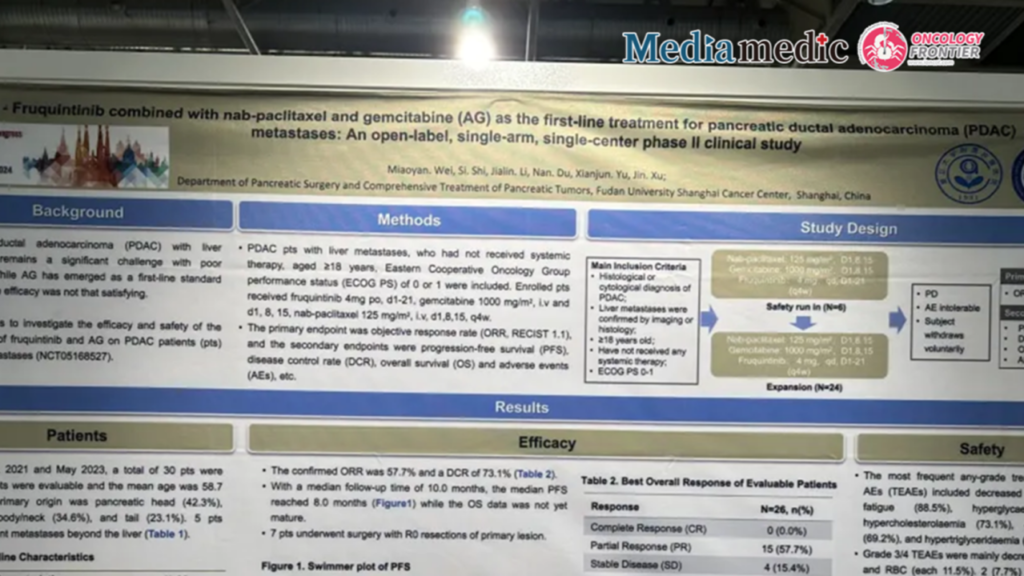
Editor's Note: The 2024 European Society for Medical Oncology (ESMO) Congress took place in Barcelona, Spain, from September 13 to 17. During the event, Dr. Miaoyan Wei from Fudan University Shanghai Cancer Center presented the results of an open-label, single-arm, single-center Phase II clinical trial exploring the use of fruquintinib combined with nab-paclitaxel and gemcitabine (AG) as a first-line treatment for liver metastases in pancreatic ductal adenocarcinoma (PDAC). This study was featured in the poster session (Abstract #1529P). In this interview, Dr. Wei provides an in-depth analysis of the study's findings.Expert Commentary
In recent years, despite progress with first-line chemotherapy regimens such as NALIRIFOX (5-FU/LV + oxaliplatin + liposomal irinotecan), (m)FOLFIRINOX (5-FU/LV + oxaliplatin + irinotecan), and AG (nab-paclitaxel + gemcitabine) in improving survival for advanced pancreatic cancer patients, the median overall survival (OS) remains less than one year, and the prognosis is poor. Researchers have continuously explored new treatment options, including combining current chemotherapy regimens with targeted therapies and/or immunotherapy. Anti-angiogenic drugs, which aim to inhibit tumor growth and metastasis by blocking angiogenesis, have been a key area of focus. Anti-angiogenic strategies for pancreatic cancer have ranged from the monoclonal antibody bevacizumab, which targets vascular endothelial growth factor (VEGF), to various “tinib” agents. Unfortunately, previous studies combining bevacizumab with gemcitabine or other chemotherapies have not significantly extended survival in advanced pancreatic cancer patients.
Unlike other tumors, where bevacizumab has notably improved survival and progression-free survival (PFS), its efficacy in pancreatic cancer may be limited due to the unique biology of this cancer. Factors include the dense stromal microenvironment, difficulty in drug delivery, and the presence of non-VEGF-dependent angiogenesis pathways. Moreover, pancreatic cancer vasculature typically exhibits high vessel density but poor functionality, which may further limit the effectiveness of anti-angiogenic therapies.
Fruquintinib, a small-molecule oral tyrosine kinase inhibitor developed in China, selectively inhibits VEGFR-1/2/3 with high kinase selectivity and binding affinity. It has already garnered high-level evidence and approval for use in advanced colorectal and gastric cancers. This study, a small-sample Phase II trial, explored the efficacy of AG combined with fruquintinib in patients with liver metastases from pancreatic cancer. Among the 30 participants, the objective response rate (ORR) was 57.7%, and the disease control rate (DCR) was 73.1%. The median follow-up period was 10 months, with a median PFS of 8 months, and seven patients successfully underwent conversion therapy with synchronous resection. Common adverse events included neutropenia and fatigue, while severe adverse events included myelosuppression and gastrointestinal bleeding.
The study suggests that anti-angiogenic therapies may be more effective in the liver metastasis subset of pancreatic cancer patients. In addition to blocking angiogenesis, such therapies may reduce the number of immunosuppressive cells, improve the tumor microenvironment, and increase the sensitivity of this patient subgroup to treatment. Combining anti-angiogenic drugs with immunotherapy on top of chemotherapy could, therefore, offer unique benefits for these patients. The IMpower150 study previously found that combining immunotherapy with anti-angiogenic drugs showed higher ORR and longer-lasting responses in patients with liver metastases from non-small cell lung cancer (NSCLC). However, these findings need further validation in broader clinical practice.
At Fudan University Shanghai Cancer Center’s Comprehensive Pancreatic Cancer Treatment Unit, where I work, we are conducting several new drug clinical trials targeting liver metastases in pancreatic cancer, using an “all in” approach combining chemotherapy with targeted and immune therapies to prolong progression-free survival.
Anti-angiogenic drugs remain a promising therapeutic target. In the future, new combination strategies will be explored, treatment approaches will be optimized, and subgroups most likely to benefit from these therapies will be identified. Overall, first-line treatment for advanced pancreatic cancer requires more innovative clinical research and treatment regimens. Additionally, incorporating high-throughput sequencing technologies to molecularly profile tumors—including genomics, proteomics, and metabolomics—will help identify new biomarkers to guide personalized treatment and improve patient outcomes.
Dr. Miaoyan Wei Fudan University Shanghai Cancer Center, Pancreatic Surgery/Comprehensive Pancreatic Tumor Treatment Unit MD in Surgery, PhD in Oncology, Visiting Scholar at MD Anderson Dr. Wei’s main research interests include the pathogenesis and comprehensive treatment of pancreatic cancer and neuroendocrine tumors. She is currently involved in several clinical drug trials and is dedicated to public health education and cancer prevention for gastrointestinal malignancies. Dr. Wei is the recipient of the Youth Fund of the National Natural Science Foundation of China and the Clinical Postdoctoral Project of Fudan University Shanghai Cancer Center.