
In January 2024, a study led by Professor Ting Niu from West China Hospital, Sichuan University was published in the international academic journal ——Frontiers In Oncology. The title of the study is “Daratumumab-based immunotherapy vs. lenalidomide, bortezomib and dexamethasone in transplant-ineligible newly diagnosed multiple myeloma: a systemic review“. This meta-analysis study represents a significant step forward in understanding the optimal treatment approaches for TIE-NDMM patients, the field remains ripe for further exploration and innovation.
Multiple myeloma (MM), a malignant clonal plasma cell disorder, represents the second most prevalent hematologic cancer globally. Its incidence notably increases with age, contributing to a growing population of elderly MM patients who are often ineligible for autologous hematopoietic stem cell transplantation (ASCT) due to poor physical condition or comorbidities. Although ASCT following effective induction therapy remains the gold standard for younger, newly diagnosed MM (NDMM) patients to enhance survival outcomes, there is a critical gap in consensus on the optimal treatment for older, transplant-ineligible NDMM (TIE-NDMM) patients. This population faces unique treatment challenges, including a heightened sensitivity to adverse events and a need for therapies that balance efficacy with tolerability. Hence, a comprehensive comparison of first-line treatment options for TIE-NDMM patients is urgently required to inform clinical practice and improve patient outcomes.
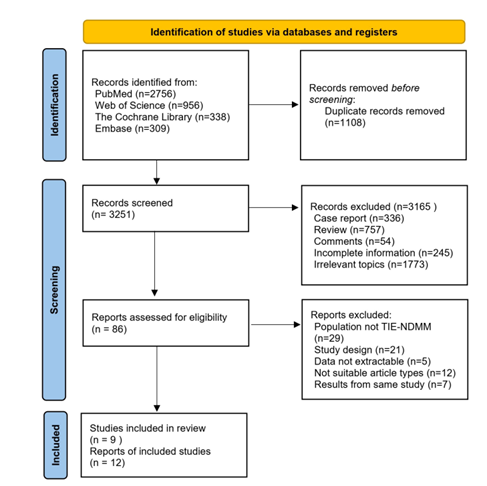
This systematic review and meta-analysis rigorously evaluated the efficacy and safety of immunotherapy using daratumumab versus the conventional regimen of lenalidomide, bortezomib, and dexamethasone (RVD) for the treatment of TIE-NDMM. We conducted a thorough search of several databases, including the Cochrane Library, PubMed, Embase, and Web of Science, to identify prospective clinical trials that compared these treatment modalities. The inclusion criteria were broad, encompassing studies on TIE-NDMM patients of any age, gender, nationality, ethnicity, and clinical stage, where the treatment involved either a daratumumab-based regimen or the RVD/RVD-lite. Critical to our analysis was the requirement for studies to report on a predefined set of endpoints crucial for assessing treatment effectiveness and safety, such as overall response rate (ORR), stringent complete remission (sCR), progression-free survival (PFS), overall survival (OS), and treatment-related discontinuation rates. Our rigorous data extraction process aimed at minimizing bias and ensuring the reliability of our findings.
(Front Oncol,2024 Jan 25:14:1286029. )
Our comprehensive analysis included data from nine prospective clinical trials, encompassing a total of 1795 patients with TIE-NDMM or NDMM lacking immediate plans for ASCT. The treatment cohorts consisted of 938 patients receiving daratumumab-based immunotherapy and 857 patients treated with RVD/RVD-lite regimens. Notably, the analysis revealed that daratumumab-based treatments significantly outperformed RVD/RVD-lite in achieving higher CR/sCR rates (47% vs. 24%, respectively; P<0.01) and longer median PFS (52.6 months vs. 35.1 months; Hazard Ratio [HR] 0.77, 95% Confidence Interval [CI], 0.66-0.90). Despite these advantages, the comparison of OS between the two treatment groups did not show a statistically significant difference (HR 1.03, 95% CI, 0.86-1.23), suggesting that both treatments ultimately provide comparable life expectancy benefits. However, the daratumumab-based regimen demonstrated a significantly lower rate of treatment-related discontinuations due to adverse events (7% vs. 16% in the RVD/RVD-lite group; P=0.03), highlighting its superior safety profile.
In summary, while the current meta-analysis represents a significant step forward in understanding the optimal treatment approaches for TIE-NDMM patients, the field remains ripe for further exploration and innovation. Future studies should aim not only to corroborate these findings but also to explore the integration of new therapeutic agents, combinations, and treatment strategies to continually improve the care and prognosis of patients with MM.


