In the ever-evolving world of medicine, the ultimate goal has consistently been to enhance patient adherence and improve treatment outcomes. This is particularly apparent in the management of HIV, where antiretroviral therapy (ART) has been the cornerstone of treatment for many years. However, with the development of long-acting ART, there has been a dramatic shift in the landscape of HIV management. This comprehensive article delves into a detailed analysis of the real-world adherence and persistence of Cabotegravir + Rilpivirine Long-Acting (CAB+RPV LA) compared to oral ART among people living with HIV (PWH) in the United States. This analysis is based on the ABOVE Study, conducted by a team of researchers and healthcare professionals from ViiV Healthcare and Analysis Group, Inc.
The Importance of Adherence in HIV Management
One of the critical aspects of HIV treatment is maintaining optimal adherence to antiretroviral therapy. Suboptimal adherence can have severe clinical and economic consequences, including loss of viral suppression, accelerated disease progression, increased mortality rates, a decrease in quality of life, and higher healthcare costs.
The game-changer in this scenario is the advent of CAB+RPV, the first guideline-recommended long-acting antiretroviral regimen approved in the U.S. for virologically suppressed PWH. This regimen has demonstrated non-inferiority to daily oral antiretroviral therapy in Phase III/IIIb studies, thus providing a promising alternative. With as few as six doses a year, CAB+RPV LA offers the advantage of less frequent dosing and directly observed therapy, which could significantly improve adherence and consequently, the success of HIV treatment.
An Overview of the ABOVE Study
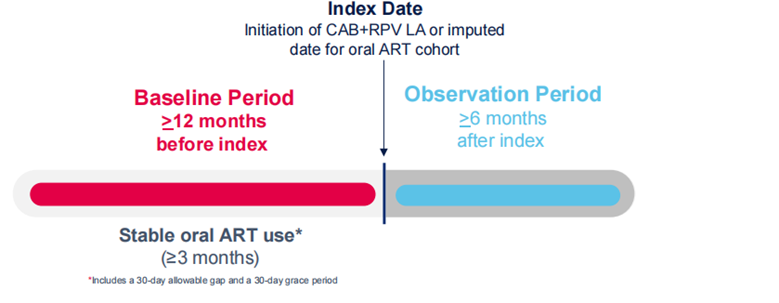
Given the recent approval and subsequent introduction of CAB+RPV LA in the medical field, the need for real-world data collection of the regimen’s effectiveness and impact in the U.S. became apparent. The ABOVE Study was initiated to fulfill this need. The study aimed to describe and compare the demographic and clinical characteristics of PWH initiating CAB+RPV LA with those remaining on oral ART. Additionally, the study sought to describe and compare adherence and persistence to CAB+RPV LA and oral ART among PWH based on the proportion of days covered (PDC).
The study design was a retrospective cohort study, utilizing administrative claims data from Symphony Health Solutions’ Integrated Dataverse. The participants of the study were PWH aged 18 or older, who were on a stable course of oral ART treatment for at least three months.
Baseline Characteristics and Their Significance
Before any adjustments were made, the CAB+RPV LA cohort was younger and had higher rates of depression, anxiety disorders, and obesity at baseline compared to the original oral ART cohort. However, after applying weighting to balance these characteristics, the cohorts were comparable, ensuring a fair comparison.
Treatment Patterns and Adherence
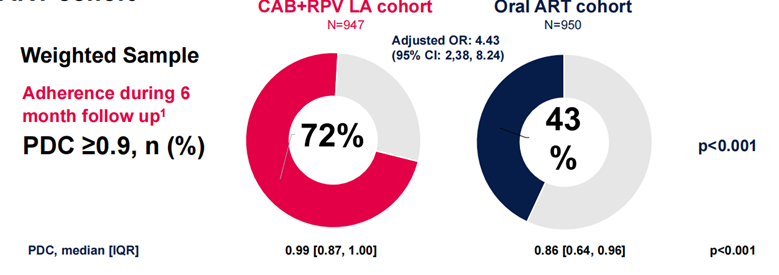
One of the key findings was that the majority of the CAB+RPV LA dosing was either conducted every two months or switched from monthly to every two months. The study found that a higher proportion of PWH in the CAB+RPV LA cohort were ≥90% adherent over a six-month follow-up compared with the oral ART cohort. Furthermore, the odds of being adherent were significantly higher in the CAB+RPV LA cohort compared to the oral ART cohort.
Persistence and Its Impact on Treatment Success
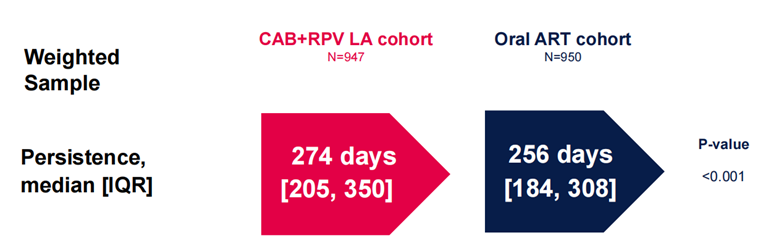
Another important aspect of treatment success is persistence, and the study revealed higher persistence with CAB+RPV LA compared to oral ART. Adherence to CAB+RPV LA remained high across all subgroups, regardless of gender, age, or insurance type. This consistency in adherence and persistence is a critical factor in long-term treatment success and overall patient outcomes.
Understanding the Limitations
While the ABOVE Study provided valuable insights, it’s essential to acknowledge certain limitations. For instance, administrative claims data may contain errors due to miscoding of medical diagnoses, leading to inaccuracies and missing data. Furthermore, despite using SMR weighting to account for potential differences between cohorts, the possibility of unmeasured confounding could not be entirely excluded. It’s also important to note that the data reflects that medications were purchased, not necessarily consumed or administered, potentially overestimating adherence or persistence status. However, this limitation is more likely to affect the oral ART cohort than the CAB+RPV LA cohort due to the nature of the treatments.
Drawing Conclusions from the ABOVE Study
Despite these limitations, the ABOVE Study yielded significant implications for HIV management. Among US PWH on stable oral ART, switching to long-acting ART resulted in significantly higher adherence and persistence. These are critical aspects of long-term success in HIV treatment, and the improvement was more pronounced when compared with those remaining on oral ART.
The study also indicated that adherence to CAB+RPV LA remained consistently high across all subgroups, i.e., gender, age, and insurance type. This consistency in adherence, regardless of demographic or economic factors, underscores the potential of CAB+RPV LA in improving treatment outcomes in a diverse population of PWH.
Long-acting ART, such as CAB+RPV LA, could be an excellent alternative to daily oral ART for PWH who could benefit from a regimen with less frequent dosing. This could include individuals who may have trouble adhering to daily medication due to lifestyle factors, cognitive issues, or simply the desire for a more manageable treatment regimen.
In conclusion, the ABOVE Study provides a valuable real-world perspective on the benefits of long-acting ART, underlining its potential to enhance adherence and outcomes in HIV management. These findings add to the growing body of evidence supporting the use of CAB+RPV LA in the management of PWH.
As healthcare professionals, it is our duty to continue exploring and supporting such innovative treatments that can significantly improve the lives of those living with HIV. The promise of CAB+RPV LA is not just in its efficacy as a treatment option but also in its potential to transform the approach to HIV management. The introduction of long-acting ART represents a significant shift from the traditional daily dosing regimen, potentially reducing the burden of daily medication intake and improving the quality of life for PWH.
Details of the Study
The ABOVE Study was a retrospective U.S. cohort study and used a robust methodology to minimize bias and ensure the accuracy of results. The participants were all PWH aged 18 or older and were on a stable course of oral ART treatment for at least three months prior to the study. This criterion was important to ensure that the participants were already familiar with and committed to an HIV management regimen, thus providing a valid comparison when they switched to CAB+RPV LA.
The researchers used Symphony Health Solutions Integrated Dataverse administrative claims data. This comprehensive database provided a rich source of information for the study but also brought with it the potential for miscoding or inaccuracies. To mitigate these issues, the researchers used SMR weighting to balance any differences between the cohorts.
The study’s objectives were clear and focused primarily on comparing adherence and persistence between CAB+RPV LA and oral ART among PWH. Adherence was measured based on the proportion of days covered (PDC), a reliable and widely used measure of medication adherence.
The Findings and Their Implications
One of the key findings from the ABOVE Study was the high level of adherence among the CAB+RPV LA cohort. Adherence to medication is a significant issue in treating any chronic condition, and this is particularly true in HIV management. The successful suppression of the virus relies on the consistent use of antiretroviral therapy. However, the burden of daily medication can be a barrier to adherence for many PWH.
The long-acting nature of CAB+RPV LA, requiring as few as six doses per year, offers a promising solution to this issue. The ABOVE Study found that a higher proportion of PWH in the CAB+RPV LA cohort were ≥90% adherent over a six-month follow-up, compared with the oral ART cohort. This high level of adherence could have a profound impact on the long-term success of HIV treatment.
Moreover, the study found that persistence, another crucial factor in treatment success, was higher among the CAB+RPV LA cohort. This further underscores the potential benefits of long-acting ART over traditional oral ART.
The study also highlighted that adherence to CAB+RPV LA remained high across all subgroups. This consistency, regardless of gender, age, or insurance type, suggests that CAB+RPV LA can be an effective treatment option for a diverse population of PWH.
Limitations, Conclusions, and Future Directions
Despite the ABOVE Study’s significant findings, it’s essential to remember that the study had certain limitations. These include potential errors in administrative claims data and the possibility of unmeasured confounding. However, these limitations do not diminish the study’s value and its implications for HIV management.
The ABOVE Study has shown that among US PWH on stable oral ART, switching to long-acting ART resulted in significantly higher adherence and persistence, compared with remaining on oral ART. This finding is an encouraging sign for the future of HIV management.
Long-acting ART, such as CAB+RPV LA, represents a significant advancement in HIV treatment. It offers a new approach for those who may struggle with the demands of daily medication, providing a more manageable and less burdensome treatment regimen. As we continue to strive for better treatments and improved patient outcomes, the findings of the ABOVE Study offer valuable insights and a promising direction for the future of HIV management.

