Recently, a breakthrough was achieved in an international multi-center real‑world study led by Professors Ji-hui Hao and Ning-ning Zhang from the Tianjin Medical University Cancer Institute & Hospital. Through a rigorous multinational clinical trial, the study demonstrated that transarterial chemoembolization (TACE) combined with atezolizumab plus bevacizumab (Ate‑Bev)confers significant survival benefits for patients with unresectable hepatocellular carcinoma (HCC)— with a median overall survival (OS) of 26.8 months versus 14.9 months in the Ate‑Bev therapy group. These findings support adoption of this regimen as a new option for advanced HCC worldwide. The study not only fills a gap in international guidelines regarding treatment strategies for advanced HCC, but also injects fresh insight into global HCC management through a “China‑led approach,”marking China’s transition from “participating in international research”to “leading global multi-center collaboration.”
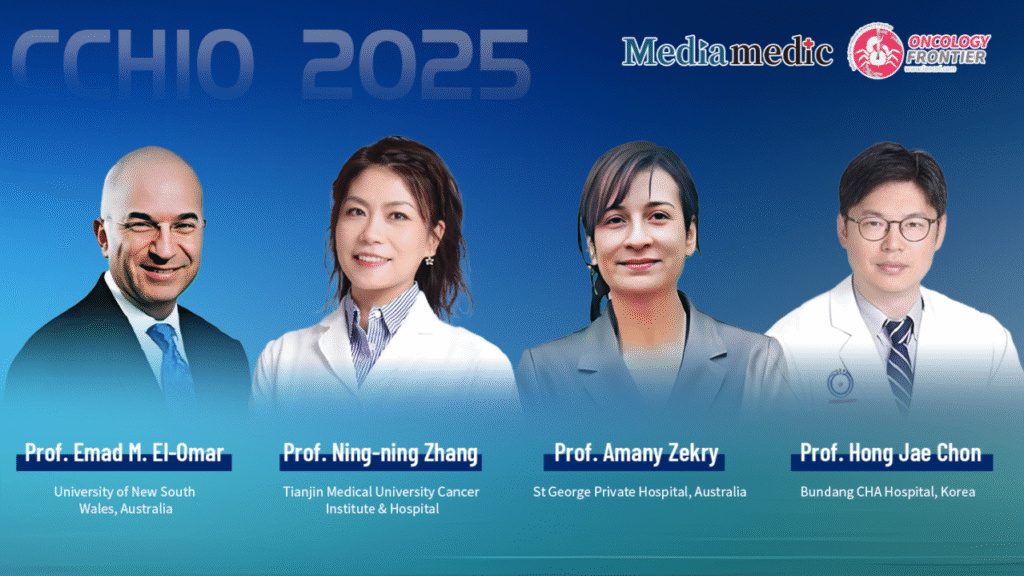
To provide an in‑depth interpretation of these groundbreaking results, The Oncology Frontier has invited the two principal Chinese investigator Prof. Ning-ning Zhang of Tianjin Medical University Cancer Institute & Hospital — together with three internationally renowned HCC experts:
- Prof. Amany Zekry (St George Private Hospital, Australia)
- Prof. Emad M. El‑Omar (University of New South Wales, Australia)
- Prof. Hong Jae Chon (Bundang CHA Hospital, Korea)
Together, they will discuss the strategic scientific value of the study, its key findings, and global implications, while also envisioning future collaboration in HCC clinical research — with the ultimate goal of enhancing survival outcomes for HCC patients around the world.
China Leading Global Collaboration — A Shift from Following to Innovating
Oncology Frontier:
As a China-led international multicenter study comparing TACE + Ate-Bev with Ate-Bev alone, what is the core value of this research in advancing global HCC treatment?
Prof. Jihui Hao:
This China-initiated international real-world study carries major clinical significance. More than 50% of global HCC cases occur in China, with hepatitis B being the predominant etiology—very different from Western countries. Existing international treatment frameworks lack tailored strategies for many subgroups of unresectable HCC, especially those with portal vein tumor thrombus (PVTT) or marginal liver function. Consequently, a large proportion of patients have no suitable standard treatment.
Relying on China’s vast clinical resources, we developed a distinctive strategy of TACE combined with systemic therapy, and through rigorous multicenter study design, successfully transformed this into high-quality global evidence. This provides the world with a China-originated, evidence-based treatment option and fills a critical gap in international guidelines.
This study marks China’s transition from collecting data as a participant to designing, leading, and validating innovative treatment strategies that influence global standards—ensuring that HCC patients worldwide benefit.
Addressing Controversy with Evidence — Study Background and Design
Oncology Frontier:
Eastern and Western guidelines differ significantly in HCC treatment. Could you describe the background, rationale, and design of this study?
Prof. Ningning Zhang:
Guideline recommendations vary widely across regions. China’s national HCC guideline—based on extensive clinical practice—lists TACE combined with systemic therapy (including Ate-Bev) as a recommended first-line therapy for unresectable HCC (CNLC IIIa).
However, major international guidelines such as NCCN, ESMO, and EASL recommend systemic therapy alone for BCLC C patients, without incorporating TACE.
Our real-world clinical experience consistently showed that TACE combined with systemic therapy might offer broader applicability and better outcomes. This raised a key scientific question: Does TACE + Ate-Bev truly provide superior survival benefit compared with Ate-Bev alone in patients with intermediate–advanced HCC?
To address this, China and France jointly designed and led an international multicenter clinical study to compare the two strategies across Asian and European populations, aiming to define a more optimized and personalized treatment approach.
Between July 2020 and December 2023, we enrolled 311 patients receiving first-line treatment for unresectable HCC. Eligibility required BCLC B/C staging, Child-Pugh A/B, ECOG 0–1, and at least one measurable intrahepatic lesion. Patients with liver transplantation, other malignancies, Child-Pugh C, or missing key data were excluded.
A total of 152 patients received TACE + Ate-Bev and 159 received Ate-Bev alone. We used inverse probability of treatment weighting (IPTW) to balance confounders such as age, cirrhosis, and PVTT. Independent radiologic review (RECIST 1.1) evaluated OS, PFS, ORR, DCR, and safety.
Breakthrough Efficacy — Major Survival Benefits
Prof. Ningning Zhang:
The results reveal a striking survival advantage.
Overall Survival (OS)
- 26.8 months with TACE + Ate-Bev
- 14.9 months with Ate-Bev
- OS extended by nearly 12 months (HR 2.66, P < 0.0001)
Progression-Free Survival (PFS)
- 16.0 months with TACE + Ate-Bev
- 6.5 months with Ate-Bev
- Significant improvement (HR 2.50, P < 0.0001)
The superiority remained robust after IPTW adjustment, confirming that the benefit was intrinsic to the strategy—not due to selection bias.
The synergy of local and systemic therapy was key: TACE rapidly debulks tumors and promotes hypoxia-induced antigen release, while Ate-Bev reshapes the tumor microenvironment and suppresses angiogenesis. Together, they create a powerful “local cytoreduction + systemic immune regulation” loop.
Safety and Expanding Indications
A major concern is whether TACE is safe for patients with PVTT or borderline liver function. This study applied precise, individualized “on-demand TACE”:
- TACE was performed only when liver function recovered to Child-Pugh A
- Imaging every ~2 months determined whether another TACE was needed
- New lesions or residual progression triggered repeat TACE
This tailored strategy ensured:
- significant tumor control, and
- no major increase in complications, including bleeding risks
Thus, even in traditionally high-risk groups (BCLC C, PVTT), TACE + Ate-Bev emerged as a safe and effective new option.
Global Impact and Future Plans
This research offers strong evidence to guide international practice. We are now collaborating with partners in France, Australia, Korea, and Japan to launch global prospective multicenter trials validating this strategy across more diverse populations (e.g., BCLC C, CNLC IIIa–IIIb). The goal is to support incorporation into global guidelines and benefit patients worldwide.
Additionally, our team has identified gut microbiome signatures associated with improved immunotherapy response. Based on this, we are planning a trial of precision microbiota transplantation to enhance immunotherapy effectiveness—one of our ambitious long-term goals.
International Experts’ Commentary
Prof. Amany Zekry:
The results are compelling. TACE converts “cold tumors” into “hot tumors,” enhancing immune recognition. The synergy between embolization and immunotherapy is biologically sound and clinically promising. Expanding this approach to non-responders, advanced BCLC stages, or patients with PVTT deserves systematic study.
Australia and China are both key HCC centers with distinct etiologies—combining our cohorts could answer many unresolved scientific questions. I look forward to deep collaboration with China and Tianjin Medical University Cancer Institute.
Prof. Hong Jae Chon:
The survival efficacy is remarkable and far exceeds what we typically see with TACE or Ate-Bev alone. Although this is retrospective, if validated prospectively, it could change clinical practice and offer patients a valuable alternative.
China and Korea share similar HCC characteristics. I am eager to work with Chinese teams—especially Tianjin—to explore optimized strategies across diverse populations.
Prof. Emad M. El-Omar:
I am honored to participate. I have a long history of collaboration with China and great admiration for China’s science and infrastructure. Tianjin Medical University Cancer Institute is one of my preferred partners.
China is poised to lead the future of cancer research, and we look forward to deepening our joint efforts to conquer cancer together.



