ZNF618::NUTM1-rearranged B-cell lymphoblastic leukemia (B-ALL) is recognized as a rare but favorable subtype of pediatric leukemia. However, this new case report published in Blood Science challenges that prognostic certainty, documenting a 3-year-old patient whose disease proved resistant to conventional chemotherapy, multiple CAR-T therapies, and hematopoietic stem cell transplantation. The findings underscore the need to reassess expectations surrounding NUTM1 fusion-positive leukemias and investigate the biological complexity behind treatment failure.Case Description and Diagnostic Workup
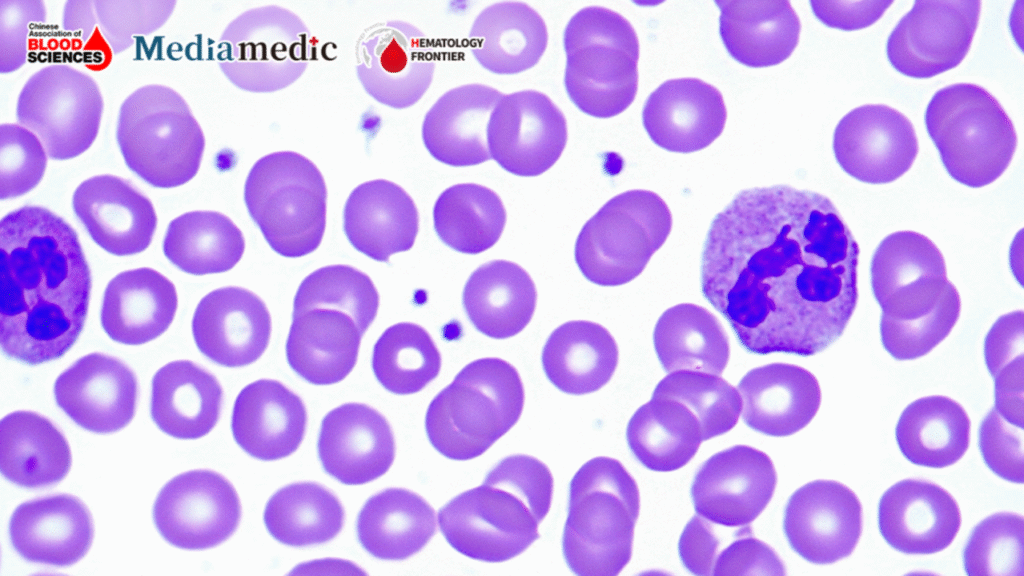
A 3-year-old boy presented with fever and was diagnosed with B-ALL based on 70% lymphoblasts in the bone marrow and flow cytometry findings. Standard screening for 41 common leukemia fusion genes and FISH analysis for multiple rearrangements were negative. Chromosomal karyotyping showed a normal profile. The child achieved complete remission (CR) after induction chemotherapy with vincristine, daunorubicin, L-asparaginase, and prednisone, followed by four consolidation courses. However, he relapsed 11 months later.
At relapse, the bone marrow showed 98.5% lymphoblasts. A new cytogenetic finding emerged: a deletion on chromosome 6q13q23. Additional next-generation sequencing of 300 leukemia-related genes revealed no pathogenic mutations, prompting further transcriptomic analysis.
Therapeutic Course and Outcomes
The patient underwent reinduction therapy but remained refractory. He then received autologous CD19-CAR T-cell therapy, which also failed. Despite further treatments—including dual-targeted CD19/CD22 CAR-T, blinatumomab with cytarabine, and allogeneic hematopoietic stem cell transplantation (allo-HSCT)—the disease relapsed again.
Post-transplant, the patient briefly achieved CR but developed severe grade IV graft-versus-host disease (GVHD). Molecular chimerism analysis revealed a loss of recipient-specific HLA genes, suggesting leukemic cells had acquired immune evasion. Treatment was eventually discontinued due to therapeutic failure and complications.
Molecular Characterization of the Fusion
Whole transcriptome sequencing identified a ZNF618 (exon 10)::NUTM1 (exon 2) in-frame fusion. This novel fusion preserved both NUT domains and resulted in high overexpression of NUTM1, confirmed through RT-PCR and Sanger sequencing. Analysis of over 1000 pediatric B-ALL cases and healthy controls showed that the fusion transcript was uniquely associated with elevated NUTM1 expression. BMI1 was also overexpressed but not uniquely to this patient, indicating it may be a common downstream effect of NUTM1 fusions.

(Blood Science. 7(2):e00230, June 2025.)
Discussion and Implications
This case contradicts the prevailing view that NUTM1-rearranged B-ALL, including those with ZNF618 partners, always carries a favorable prognosis. It is one of the few reported cases of poor outcome in this subtype, and the first involving ZNF618::NUTM1 with aggressive progression despite multimodal treatment.
Several possible resistance mechanisms were explored. The 6q13q23 deletion may have contributed to leukemogenesis via loss of tumor suppressors. Immune evasion likely played a role as well—malignant cells partially expressed PD-1, a rare finding in B-ALL, potentially affecting CAR-T efficacy. Notably, PD-L1 expression was absent, suggesting alternative pathways of immune escape. Finally, the authors highlight that epigenetic dysregulation—such as altered DNA methylation or chromatin remodeling—might affect gene expression, immune resistance, and leukemic stemness.
These findings emphasize the need to re-evaluate the prognostic assumptions about ZNF618::NUTM1 fusions and encourage deeper genomic and epigenetic profiling in treatment-resistant B-ALL cases.
Conclusion
This case illustrates that not all NUTM1-rearranged B-ALLs follow a favorable clinical course. The presence of ZNF618::NUTM1, even with otherwise unremarkable molecular findings, may portend a worse prognosis in some instances. Clinicians should approach this fusion with caution, and researchers are encouraged to investigate its biological role more thoroughly. Molecular and immune profiling—including epigenetic analysis—may be key to understanding and overcoming therapeutic resistance in future cases.
Click the link to view the original article:


