
In January 2024, a study led by Professor Gang An from Institute of Hematology & Blood Diseases Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College was published in the international academic journal ——American Journal of Hematology(IF=12.8). The title of the study is “Development and validation of an individualized and weighted Myeloma Prognostic Score System (MPSS) in patients with newly diagnosed multiple myeloma“. This study represents a significant leap forward in precision medicine for multiple myeloma (MM).
The research spearheaded by Gang An and his team involved a meticulous process of data collection and analysis. The study retrospectively reviewed clinical and genetic information from 1792 patients newly diagnosed with MM across various institutions. This broad patient base ensured the study’s findings would be robust and applicable to a wide demographic. The researchers employed advanced statistical tools to sift through this wealth of data, identifying the most predictive features for overall survival (OS) in MM patients. This methodological rigor underpins the study’s credibility and the reliability of the MPSS as a prognostic tool.
A pivotal element of the study was the identification of four major risk factors: elevated lactate dehydrogenase (LDH) levels, ISS Stage III, thrombocytopenia, and cumulative high-risk cytogenetic aberrations (HRA). The innovative aspect of the MPSS lies in how it assigns a weighted value to each risk factor, based on its hazard ratio for OS. This nuanced approach acknowledges the complex interplay between various prognostic indicators and their collective impact on patient outcomes.
(Am J Hematol . 2024 Jan 21. )
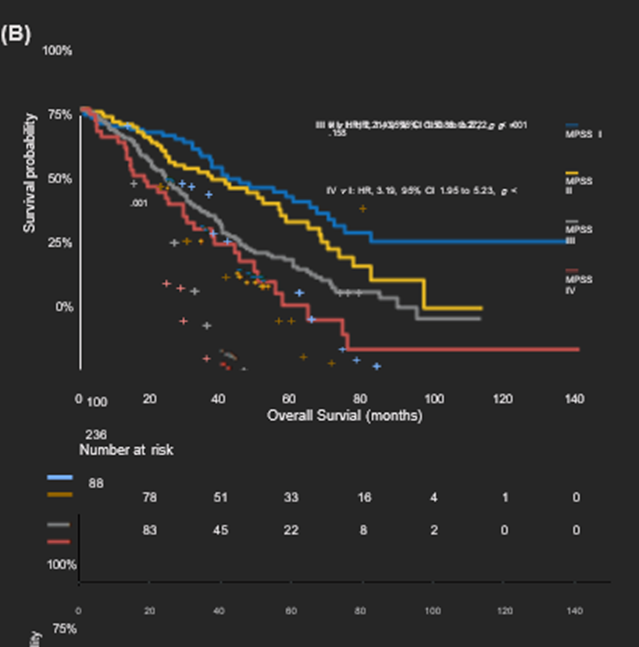
The stratification of patients into four distinct risk categories (MPSS I-IV) based on their cumulative score is a testament to the system’s granularity and precision. This stratification allows for a nuanced assessment of risk, enabling healthcare professionals to tailor treatment strategies more effectively. The validation of the MPSS, demonstrating its ability to accurately predict OS with significant discrimination between risk groups, underscores its potential as a valuable tool in clinical practice.
The introduction of the MPSS represents a significant advancement in the field of hematology, particularly in the treatment of MM. By providing a more accurate and individualized risk assessment, the MPSS enables clinicians to devise treatment plans that are better aligned with each patient’s unique prognostic profile. This individualized approach is at the forefront of precision medicine, aiming to optimize patient outcomes through tailored therapeutic strategies.
The study also opens avenues for future research, particularly in the prospective validation of the MPSS across diverse patient populations and in different clinical settings. Additionally, integrating the MPSS with emerging treatment modalities and novel therapeutic agents could further enhance its utility, potentially leading to even more personalized and effective approaches to managing MM.
In conclusion, the work of Gang An and his international team in developing the MPSS is a monumental step forward in the fight against multiple myeloma. By offering a more precise prognostic tool, the MPSS not only enhances our understanding of MM but also provides a foundation for more personalized and effective treatment strategies, heralding a new era of hope for patients diagnosed with this complex disease.


