
In November 2023, a study led by Professor XiaoFan Zhu from Chinese Academy of Medical Sciences Blood Disease Hospital (Institute of Hematology, Chinese Academy of Medical Sciences) was published in the international academic journal ——BMC Infectious Diseases. The title of the study is "Acinetobacter spp. Bloodstream Infection in Hematological Patients: A 10-Year Single-Center Study". This comprehensive study sheds light on the significant burden of Acinetobacter spp. BSI in hematological patients, emphasizing the complexity of treating these infections in a population at high risk of adverse outcomes.Acinetobacter spp. are Gram-negative bacteria that have emerged as critical pathogens in healthcare settings, causing a wide range of infections, including pneumonia, bloodstream infections (BSI), urinary tract infections, and meningitis. These organisms are particularly notorious for their ability to survive in the hospital environment and to develop resistance to multiple antimicrobial agents, complicating treatment strategies. Among the species, A. baumannii is the most prevalent and studied; however, other species within the genus, such as A. pittii and A. calcoaceticus, have increasingly been recognized for their role in nosocomial infections. The adaptability and resilience of Acinetobacter spp. pose significant challenges in managing infections, especially in vulnerable populations such as hematological patients, who are at a higher risk due to their immunocompromised state.
Beyond identifying the clinical characteristics and antimicrobial resistance patterns of Acinetobacter spp. BSI in hematological patients, this study also aims to delve into the molecular epidemiology and genotypic features of the isolates. Understanding the genetic mechanisms underlying drug resistance and pathogenicity can offer insights into the development of targeted therapeutic and preventive strategies. Moreover, evaluating the impact of infection control practices on the incidence of Acinetobacter spp. BSI in this patient population can provide valuable information for hospital policy-making and patient care protocols.
To achieve a thorough analysis, this study employed a multifaceted approach, including:
– Detailed chart reviews to gather comprehensive patient data, such as underlying hematological conditions, treatment regimens, infection onset, and outcomes.
– Microbiological identification and susceptibility testing using advanced molecular techniques to accurately characterize the isolates and determine their resistance profiles.
– Epidemiological analysis to trace the sources and transmission pathways of the infections within the healthcare setting, employing genotyping and phylogenetic studies.
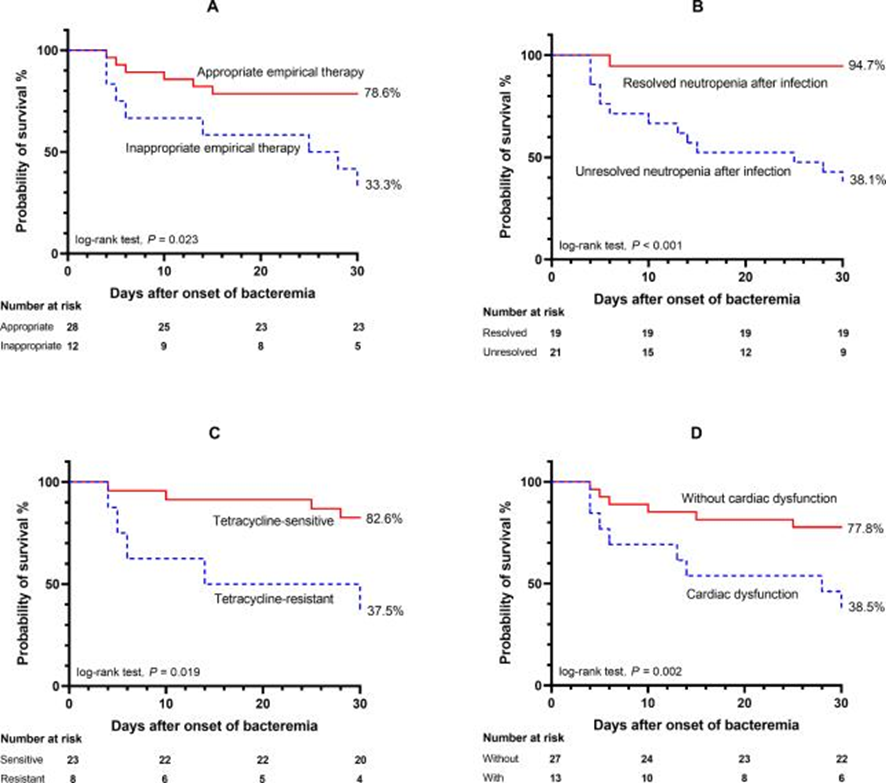
– Statistical analyses incorporating both univariate and multivariate models to identify significant predictors of outcomes, ensuring robust adjustments for potential confounders.
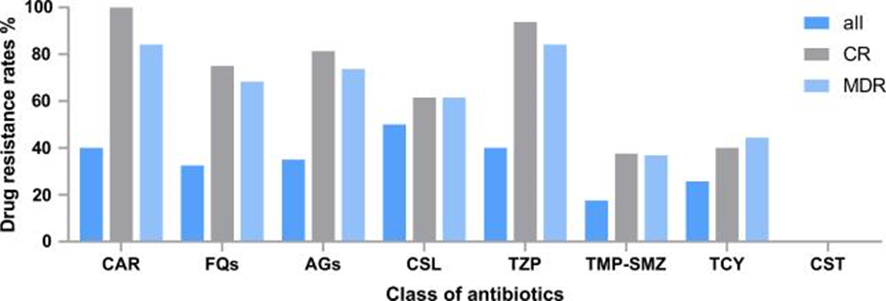
The results section provides an in-depth look at the distribution of Acinetobacter species, revealing a diverse array of strains implicated in BSIs among hematological patients. The molecular analysis indicates a high prevalence of carbapenemase-producing genes, highlighting the mechanism behind the high resistance rates to carbapenems observed in the study. The epidemiological investigation points to several nosocomial outbreaks, underscoring the importance of infection control measures in preventing the spread of these resistant organisms.
(BMC Infect Dis. 2023 Nov 14;23(1):796. )
By offering a multidimensional view of Acinetobacter spp. BSI in hematological patients, this study contributes valuable insights into the epidemiology, clinical management, and prevention strategies for these infections. It underscores the necessity of a coordinated approach involving clinicians, microbiologists, infection control specialists, and policymakers to address the challenges posed by multidrug-resistant Acinetobacter spp. in healthcare settings.
In conclusion, this comprehensive study sheds light on the significant burden of Acinetobacter spp. BSI in hematological patients, emphasizing the complexity of treating these infections in a population at high risk of adverse outcomes. The findings highlight the urgent need for innovative approaches to diagnosis, treatment, and prevention, as well as the critical role of hospital infection control practices in managing the spread of these resistant pathogens.


